Achilles Tendinitis: Symptoms, Causes, Prevention
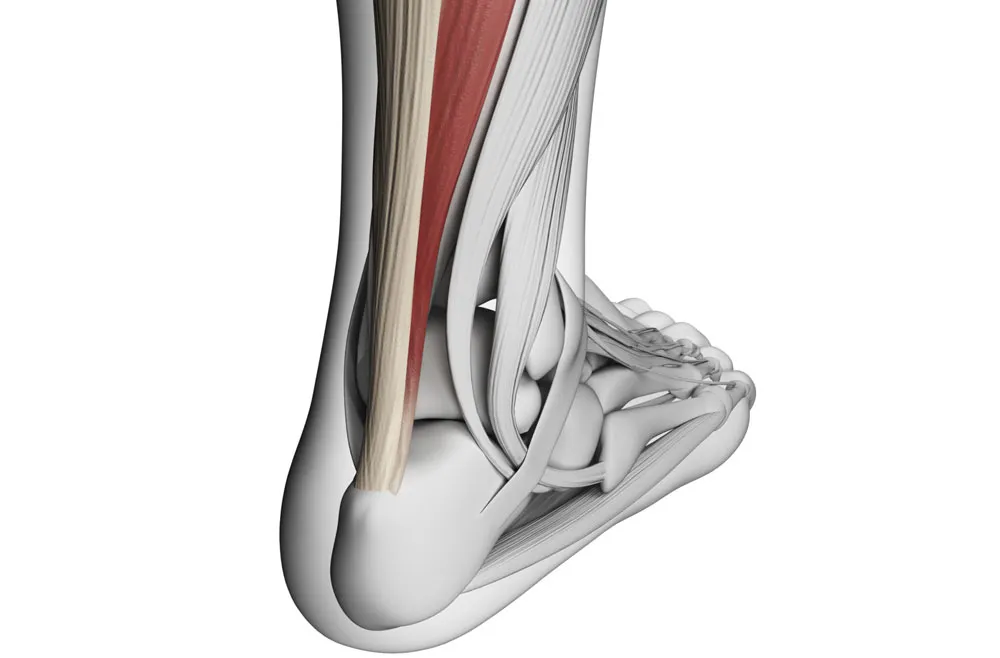
Achilles tendinitis is a prevalent overuse injury that impacts the Achilles tendon—a critical band of tissue that connects the calf muscles to the heel bone.
Nov. 13, 2023, 4 min read, Articles
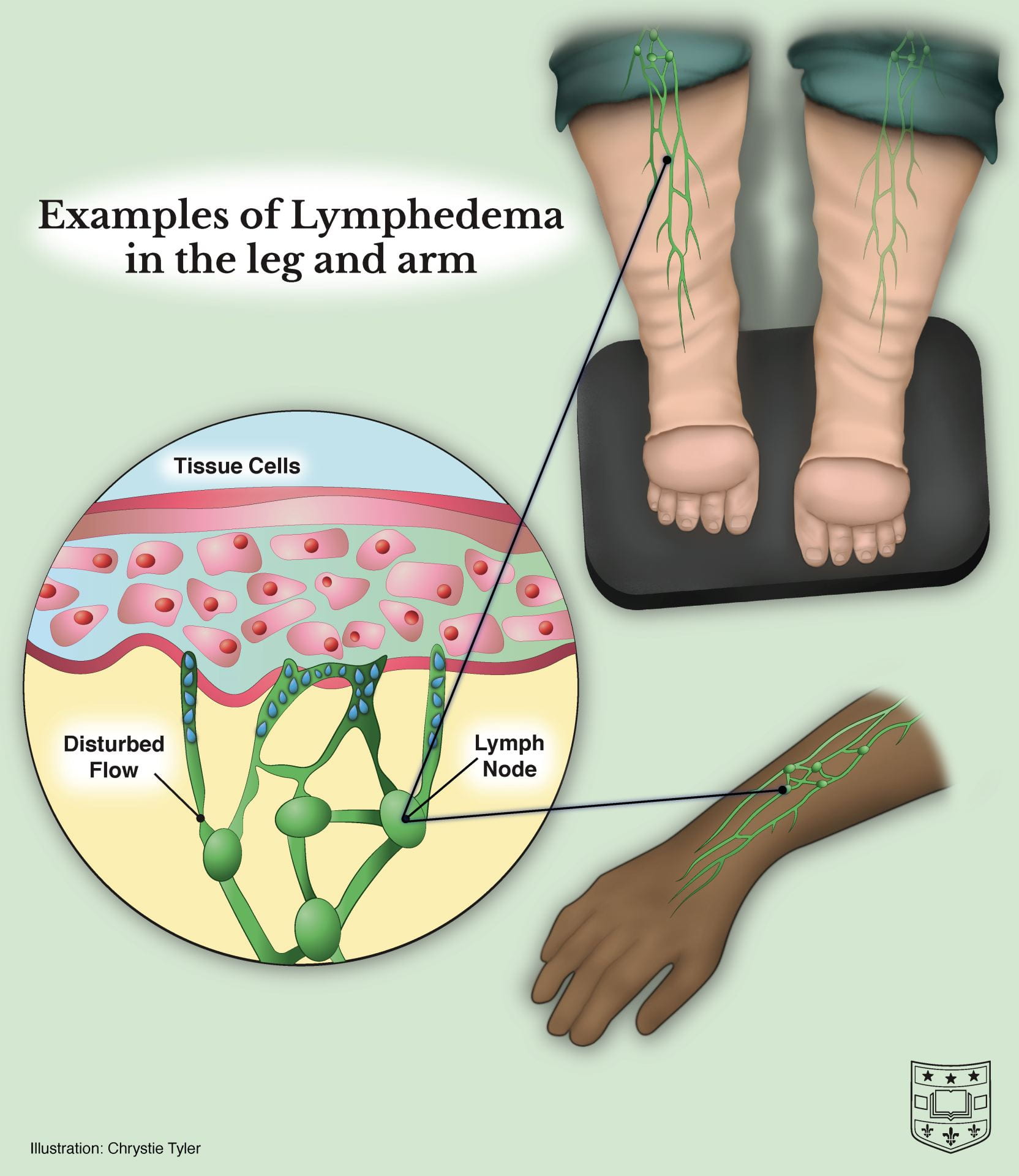
Lymphedema is a chronic condition characterized by the accumulation of lymphatic fluid, leading to persistent swelling, typically in the arms or legs. This condition arises when the lymphatic system, responsible for draining excess fluid from tissues, is compromised. Navigating the intricacies of lymphedema involves understanding its multifaceted causes, recognizing a spectrum of symptoms, and embracing effective management strategies, including innovative approaches like osteopathy and physiotherapy.
Lymphedema can be classified into two main types: primary and secondary.
This rare form of lymphedema is often hereditary, resulting from congenital malformations in the lymphatic system. Symptoms may manifest at birth, during adolescence, or later in life. Primary lymphedema can be further categorized:
More common than the primary form, secondary lymphedema occurs due to damage or obstruction of the lymphatic system. Common causes include:
The hallmark symptom of lymphedema is persistent swelling, often in the arms or legs, but it can affect other parts of the body. Other symptoms may include:
While there is no cure for lymphedema, various management strategies can help control symptoms and improve the quality of life for individuals affected.
For individuals at risk of developing lymphedema, such as cancer survivors, taking proactive measures can reduce the likelihood of its onset:
Lymphedema poses unique challenges, but with a thorough understanding of its causes and symptoms, individuals can embark on effective management strategies. Early detection, education, and a multidisciplinary approach involving healthcare professionals, including physiotherapists and osteopathic practitioners, are pivotal in ensuring effective care. As research continues to advance, there is optimism for enhanced therapeutic strategies and improved outcomes for those affected by lymphedema.
Achilles tendinitis is a prevalent overuse injury that impacts the Achilles tendon—a critical band of tissue that connects the calf muscles to the heel bone.
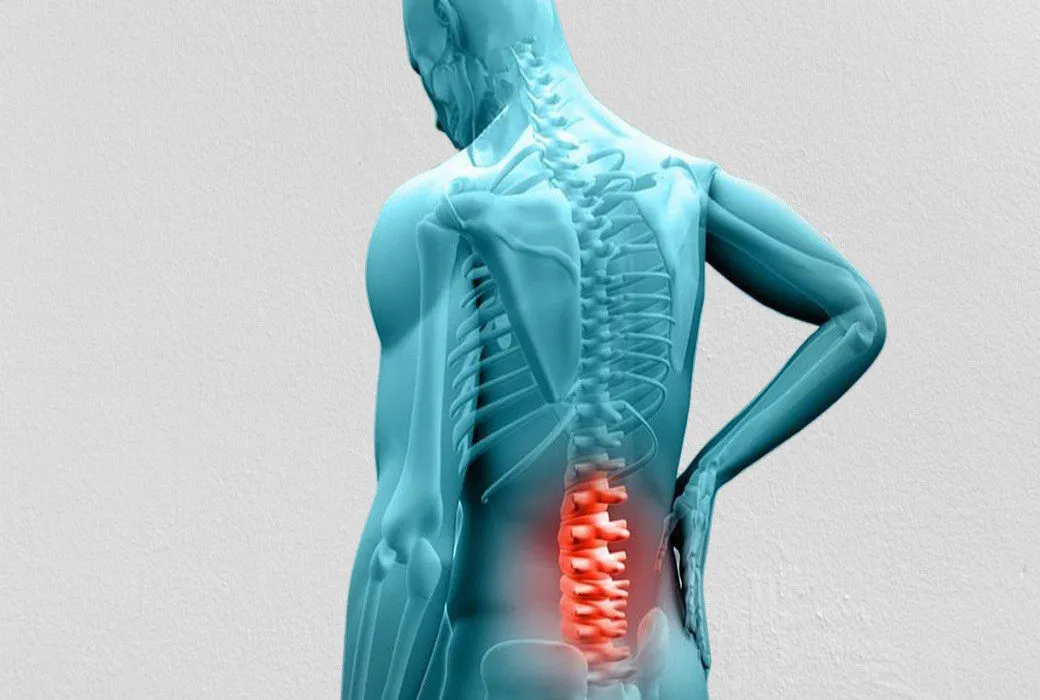
Back pain is a prevalent and often debilitating condition that can affect individuals of all ages and walks of life.

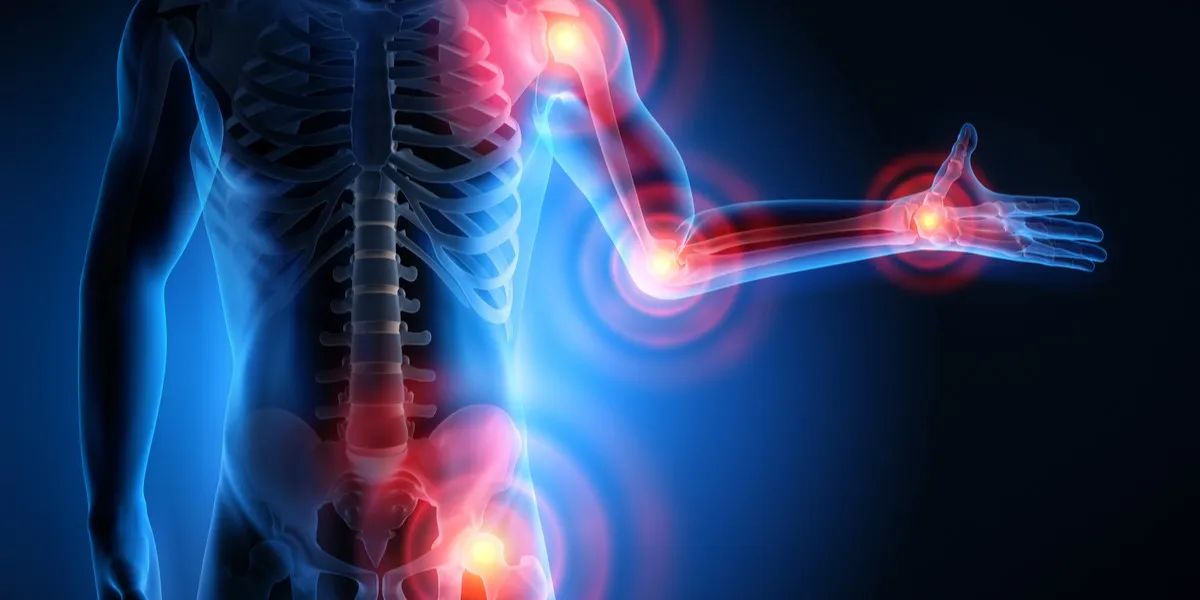
Arthritis is a common and often painful condition that affects millions of individuals worldwide. It's not a single disease but rather a group of more than 100 different types of joint-related conditions.
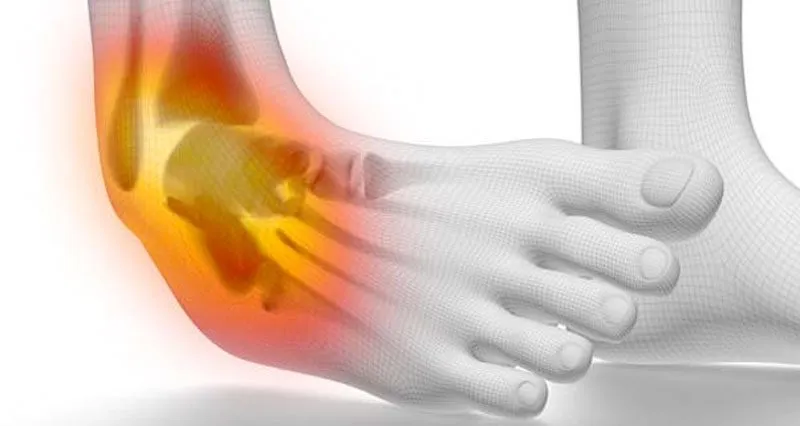
Ankle injuries are prevalent in the world of sports and can be a significant setback for athletes.
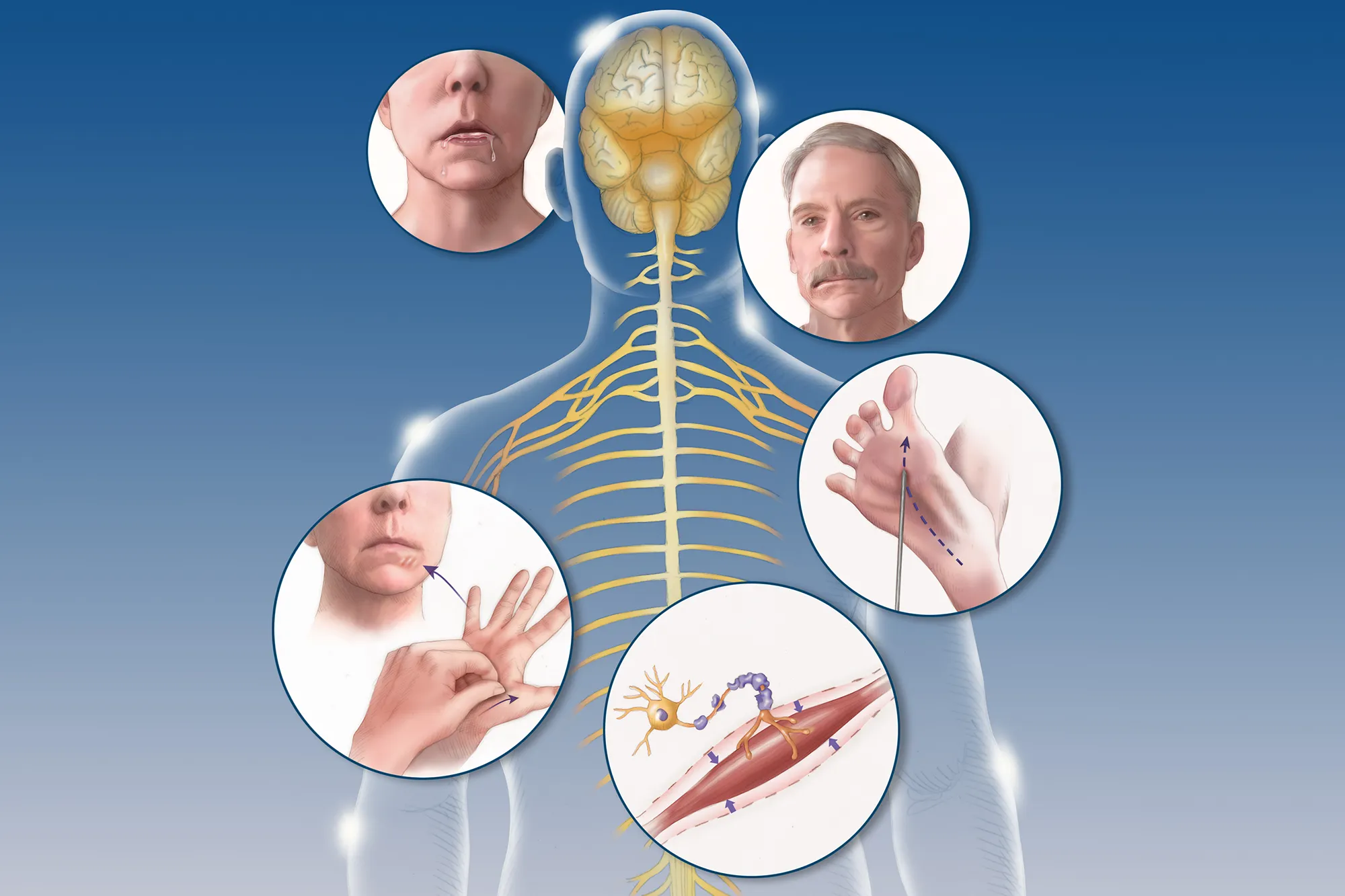
Amyotrophic Lateral Sclerosis (ALS), often referred to as Lou Gehrig's disease, is a progressive neurodegenerative disorder that affects nerve cells in the brain and spinal cord.
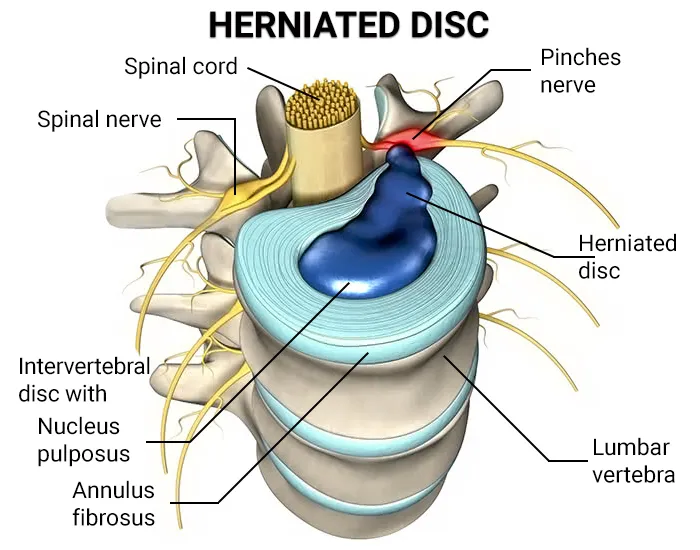
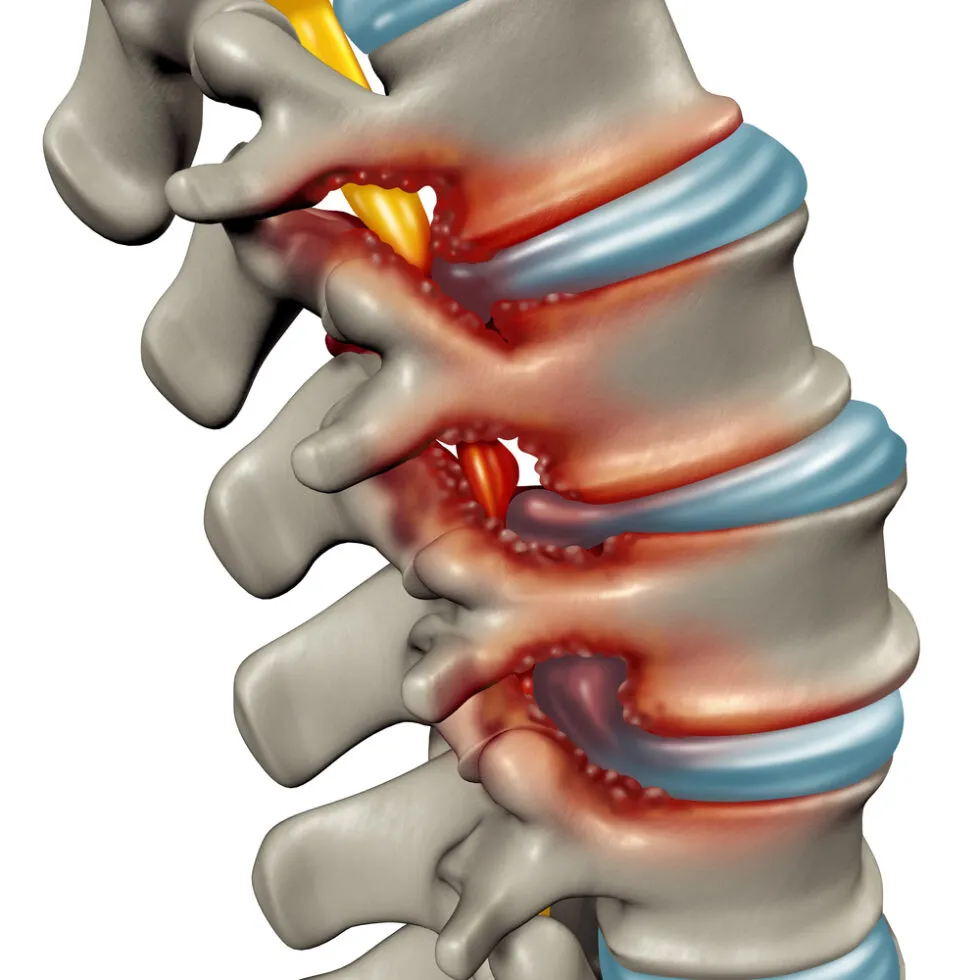
Degenerative Disc Disease (DDD) is a common condition that affects the intervertebral discs in the spine.
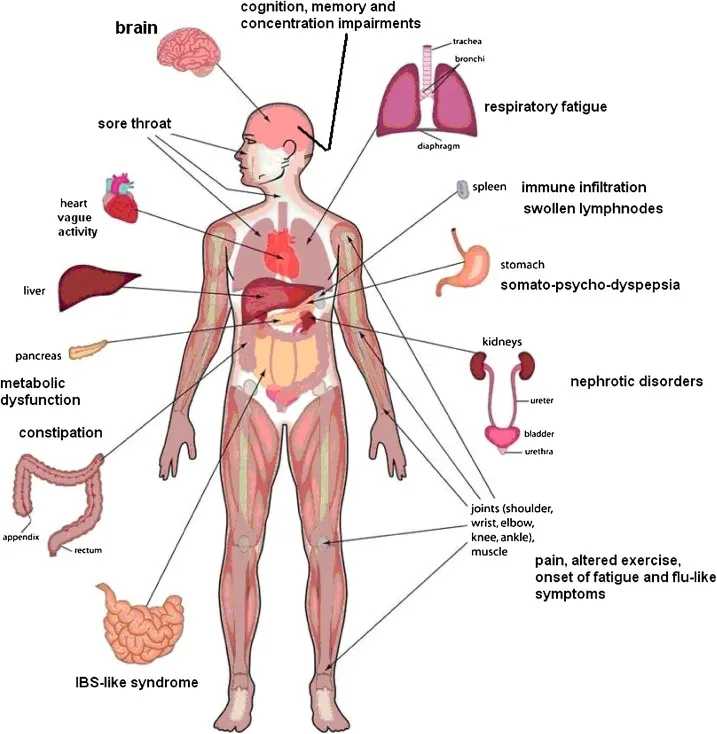
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is a perplexing and debilitating condition that impacts individuals, often altering their daily lives and challenging conventional understanding.
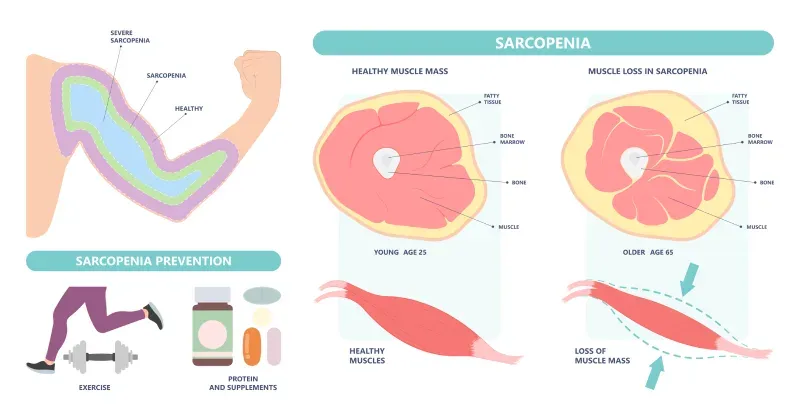
Muscular dystrophy encompasses a group of diseases leading to progressive muscle weakness and loss of muscle mass. The development of abnormal genes disrupts the production of necessary proteins crucial for healthy muscle function.

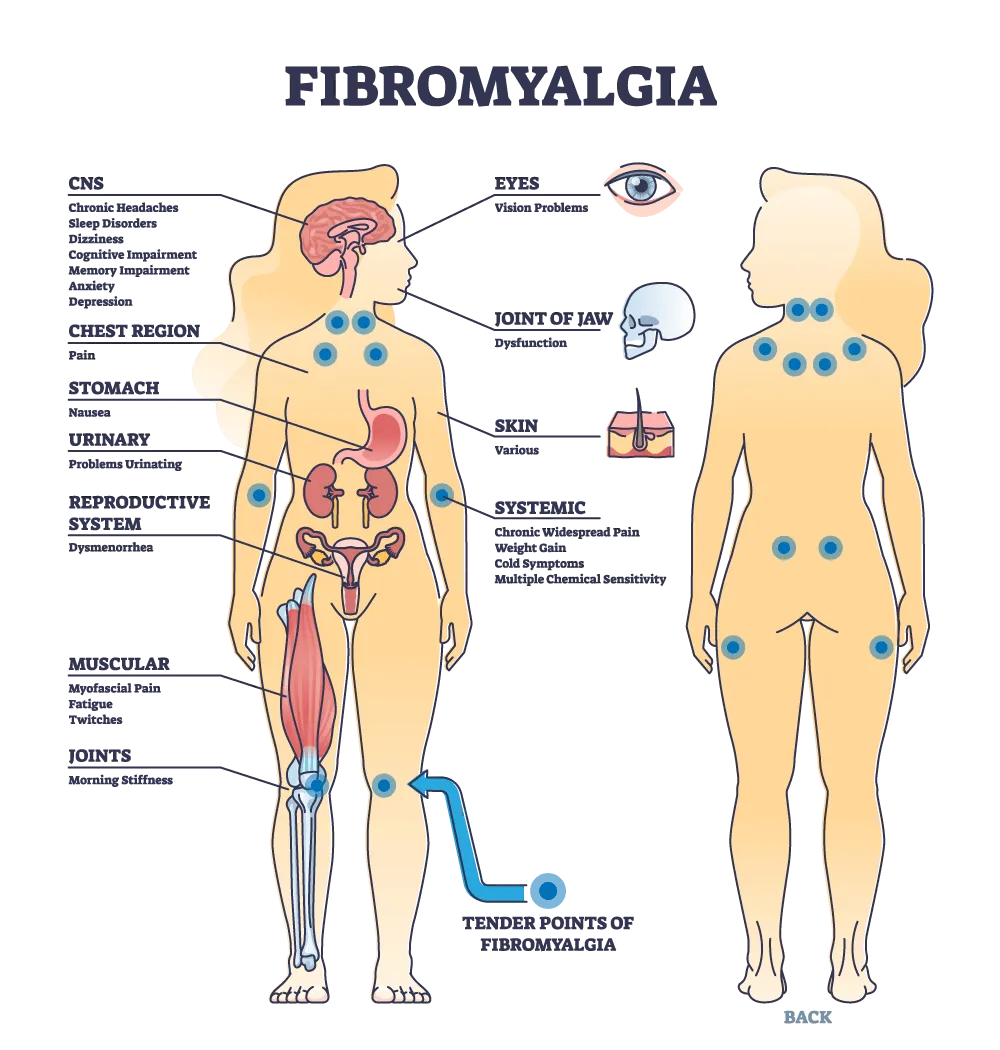
Fibromyalgia stands as a complex and often misunderstood condition characterized by widespread musculoskeletal pain, fatigue, and sleep disturbances
Bunions, medically referred to as "hallux valgus," are a common and often painful foot deformity that affects the joint at the base of the big toe.

Herniated disc symptoms can be debilitating, causing pain, numbness, and mobility limitations.
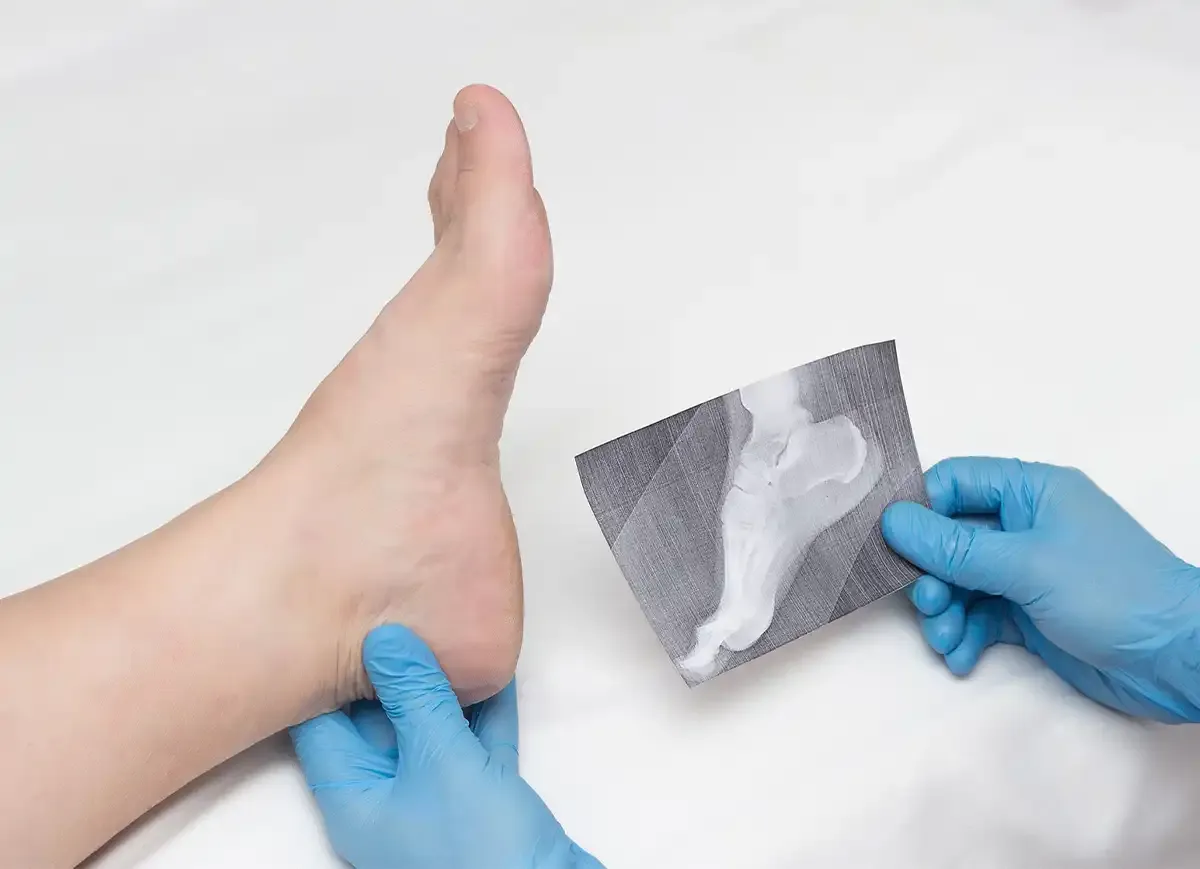
A heel spur is a bony growth that pokes out below your back heel bone inside of your foot. Heel spurs happen when stress and strain damages your foot ligaments.
Knee pain is a widespread issue that can significantly impact a person's mobility and quality of life.Knee pain is a widespread issue that can significantly impact a person's mobility and quality of life.

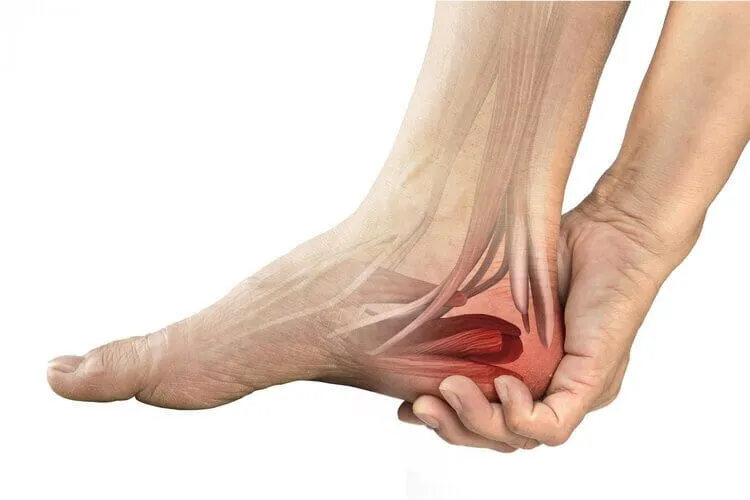
Heel pain can be a nagging and uncomfortable issue that affects many people. In this article, we will explore the various causes of heel pain, common symptoms associated with it, and the available treatments that can help you find relief and get back to your active lifestyle.
Military Neck, also referred to as Cervical Kyphosis, is a condition that affects the natural curvature of the cervical spine, resulting in the loss of its typical curve.

Migraines and headaches are prevalent neurological disorders that affect a significant portion of the population.

Plantar fasciitis is a common and often painful foot condition that affects millions of people worldwide.

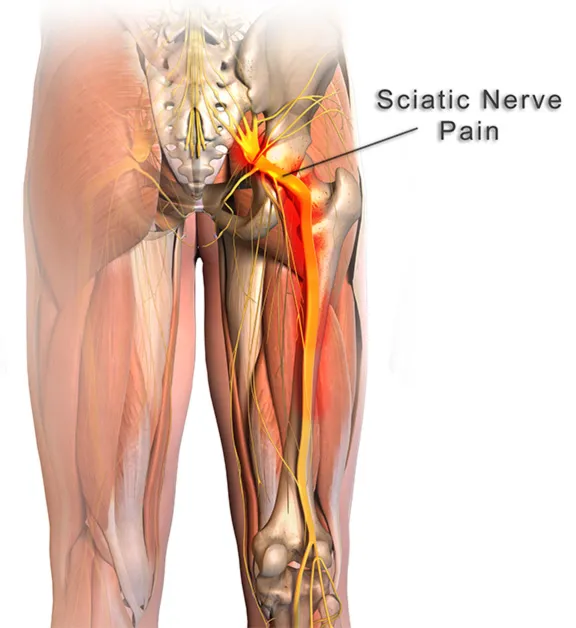
Piriformis syndrome is a perplexing condition, often overshadowed by more common sources of hip and lower back pain.

motor vehicle accidents (MVA) can result in a wide range of injuries, from minor bruises to severe trauma. in the aftermath of such incidents, seeking prompt medical attention is crucial for assessing and addressing any injuries sustained.

Sarcopenia is the gradual loss of muscle mass that can affect people in their 30s and beyond. WebMD explains its symptoms, causes, diagnosis, and treatments.
Spinal stenosis, a prevalent spinal condition, is characterized by the narrowing of the spinal canal, leading to discomfort and neurological symptoms.
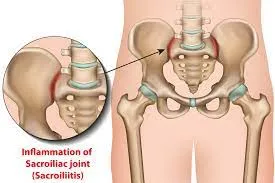
The sacroiliac joint, a crucial junction between the sacrum and the ilium bones in the pelvis, plays a pivotal role in supporting the weight of the upper body.
A rotator cuff injury can be a painful and limiting condition, impacting the functionality of the shoulder.

Suffering from lower back pain from sitting? It could be from poor ergonomics in your workplace. Learn more with these tips for how to alleviate pain from sitting.

Sciatica is a painful and often debilitating condition that affects numerous individuals worldwide.
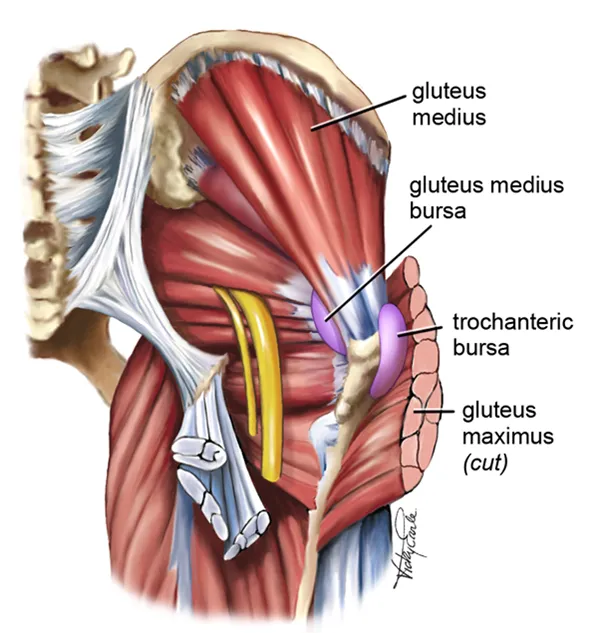
Gluteal tendinopathy is a condition that affects the tendons in the gluteal region, leading to pain and restricted mobility.
Tennis Elbow, also known as Lateral Epicondylitis, is a painful condition that affects the tendons in the forearm, causing discomfort and limited mobility in the elbow and wrist.

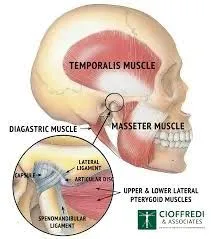
The temporomandibular joint (TMJ) serves as a pivotal mechanism, allowing us to perform everyday activities such as speaking, chewing, and yawning with ease. However, when this complex joint encounters issues, it can lead to Temporomandibular Joint Syndrome (TMJ syndrome).
Tarsal Tunnel Syndrome (TTS) is a common and often painful condition affecting the tarsal tunnel—a narrow passage in the ankle.

Explore the impact of time-restricted eating on heart health. Learn about the connection between diet and cardiovascular risk.

Most cases of foot or ankle pain are short term and are caused by soft tissue injuries, such as sprains or strains. You can usually ease the pain yourself But see York Rehab Clinic if the pain does not improve.

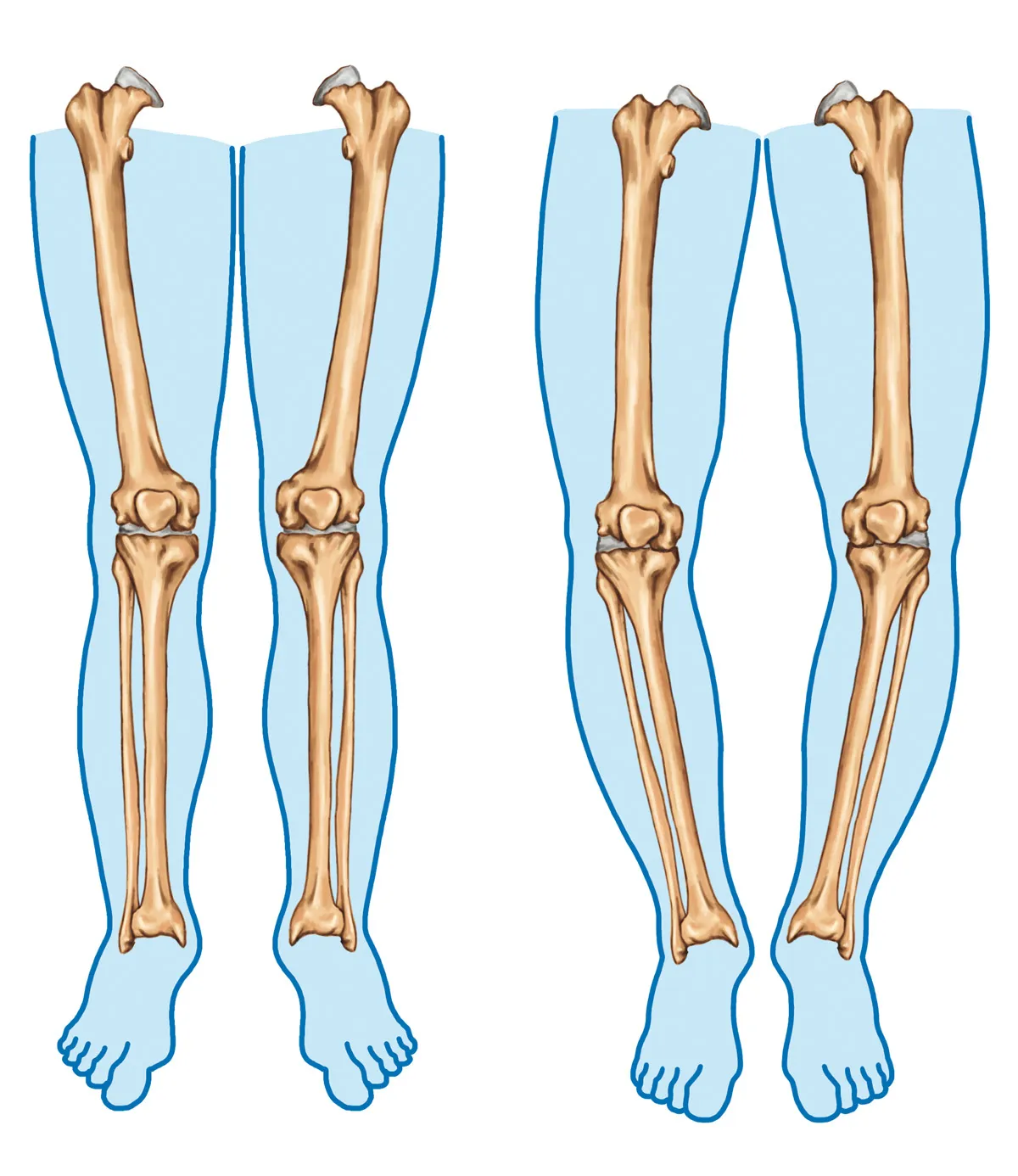
Bow legs is a genetic condition where the knees bow outward when standing. Learn its symptoms and causes at York Rehab Clinic.
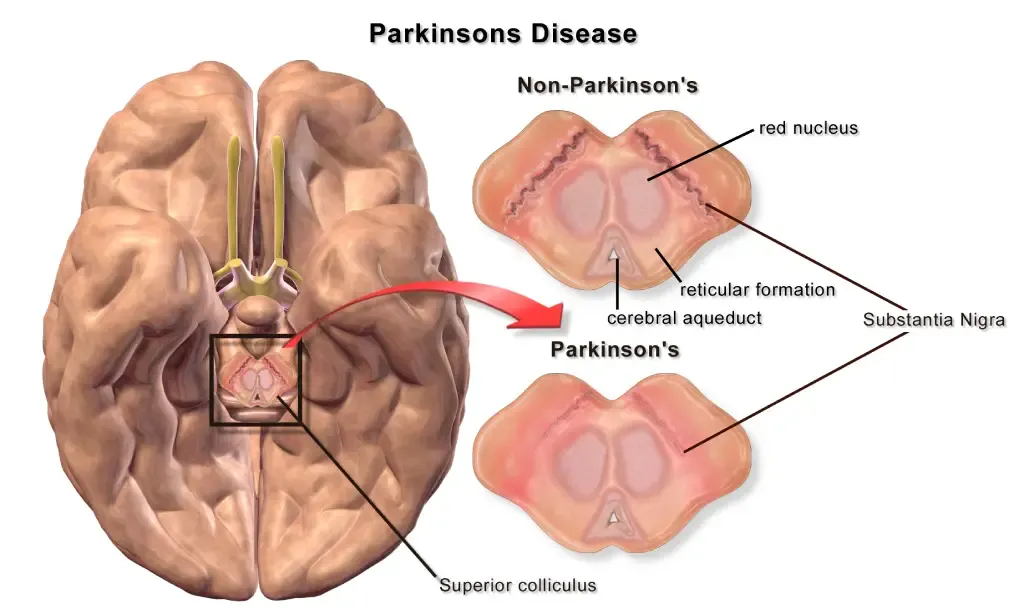
This article explores the complexities of Parkinson’s Disease and sheds light on the therapeutic benefits offered by osteopathy and physiotherapy.
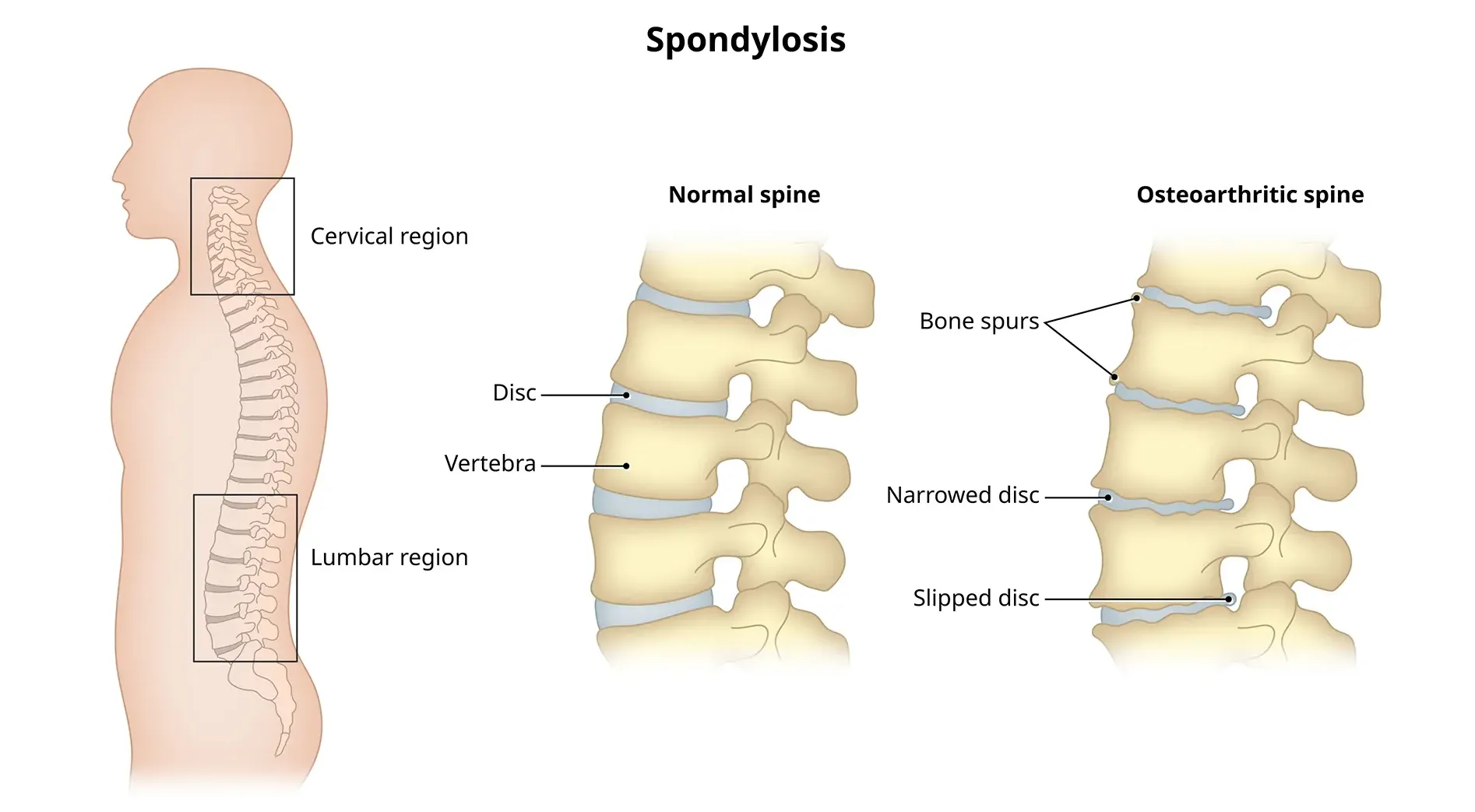
Cervical spondylosis, a prevalent condition, unfolds as a result of wear and tear on the spinal discs in the neck.
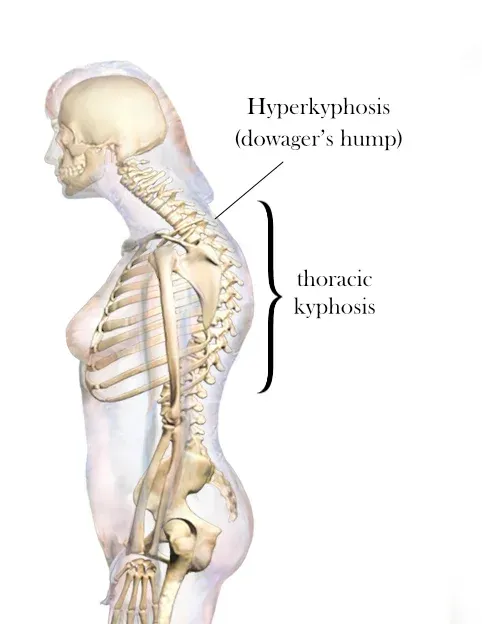
A dowager’s hump, a curve at the base of your neck, can cause extreme fatigue, back pain and headaches.
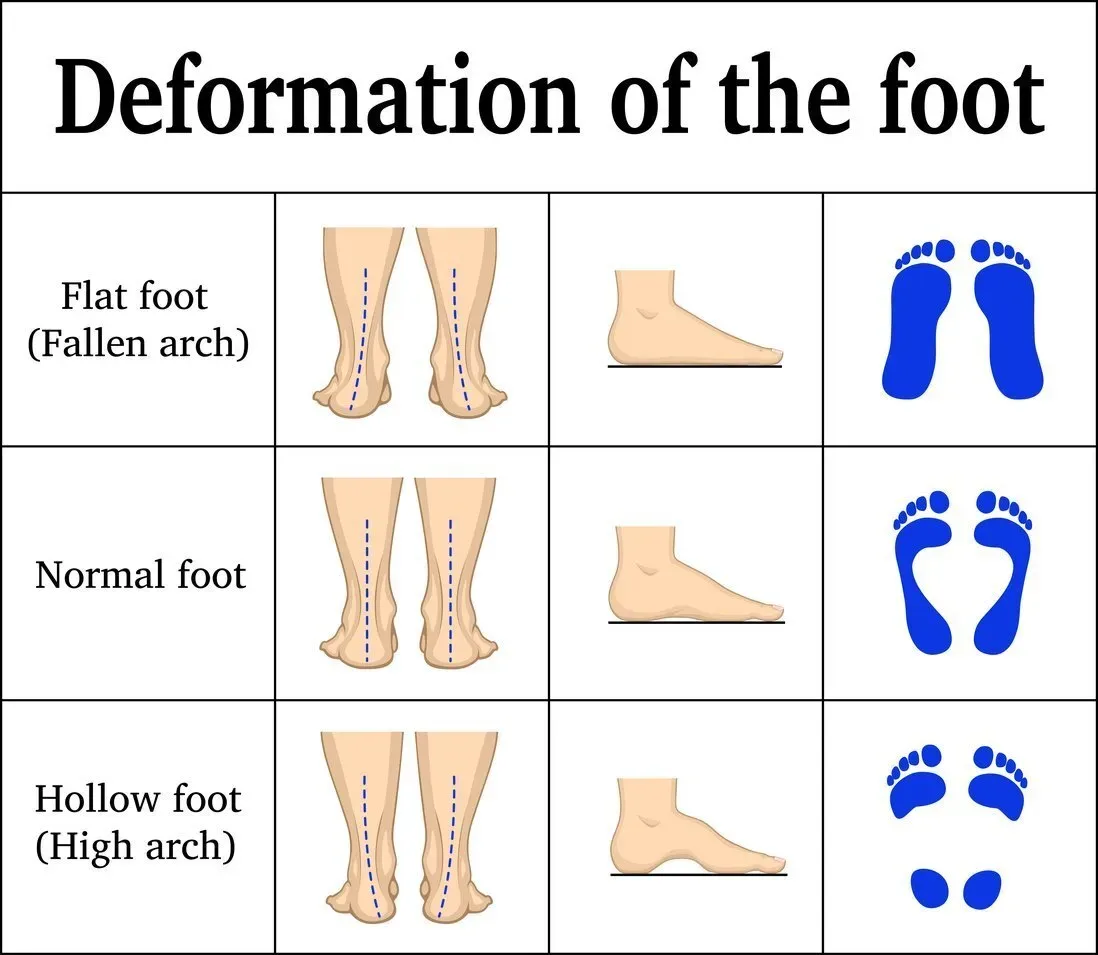
Flat feet cause pain, muscle strain, and fatigue. Treatments can ease discomfort. Symptoms include ankle pain, muscle fatigue and changes in walking.
Traumatic brain injury (TBI) often results from a violent blow or jolt to the head or body, causing various physical and psychological effects.

Introduction: Neck stiffness can be a discomforting and limiting condition that affects people of all ages.
