Achilles Tendinitis: Symptoms, Causes, Prevention
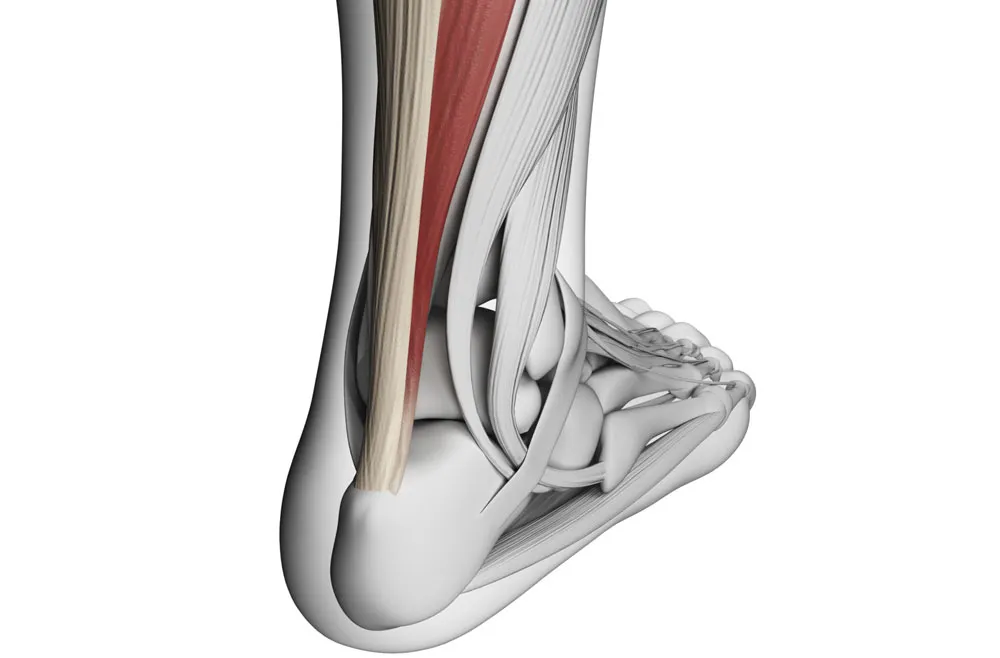
Achilles tendinitis is a prevalent overuse injury that impacts the Achilles tendon—a critical band of tissue that connects the calf muscles to the heel bone.
Jan. 17, 2024, 7 min read, Articles

Migraines and headaches, pervasive and intricate neurological phenomena, delve into the intricate landscape of cranial pain. Beyond the shared realm of discomfort, these conditions exhibit unique characteristics and implications. This overview aims to unravel the multifaceted nature of migraines and headaches, providing insights into their distinctions and the impact they wield on daily life.
Headaches encompass a diverse spectrum, from tension-type headaches characterized by a persistent, dull ache to migraines marked by intense, pulsating pain often accompanied by additional sensory symptoms.
- *Variability:* Understanding this variability is pivotal in accurate diagnosis and tailoring effective treatment plans.
- *Tension-Type Headaches:* These headaches may manifest episodically, triggered by specific stressors, or evolve into a chronic state, persisting for extended periods.
- *Migraines:* Distinguished by episodic attacks lasting hours to days, with distinct prodrome and postdrome phases, migraines introduce an added layer of complexity.
- *Tension-Type Headaches:* While often manageable, chronic tension-type headaches can impact daily functioning, influencing work, relationships, and overall quality of life.
- *Migraines:* The severe nature of migraines, accompanied by nausea, light sensitivity, and visual disturbances, can significantly disrupt daily activities, necessitating periods of rest and recovery.
- *Tension-Type Headaches:* Stress, poor posture, and muscle tension emerge as common triggers, intertwining with lifestyle factors.
- *Migraines:* A multitude of triggers, including hormonal changes, specific foods, sensory stimuli, and emotional stress, contribute to the intricate web of migraine causation.
- *Distinguishing Features:* The nuanced features of migraines and tension-type headaches hold diagnostic significance, guiding healthcare professionals in formulating targeted interventions.
- *Personalized Care:* Recognizing the individuality of each case is paramount for tailoring personalized care plans that address the unique characteristics and triggers associated with cranial pain.
In navigating the intricate landscape of migraines and headaches, this overview serves as a compass, offering a foundational understanding of their diverse manifestations. Beyond the common thread of cranial pain, recognizing the subtleties and distinctions enhances the ability to decode the complexities of these prevalent neurological conditions.
- *Description:* Tension-type headaches manifest as a continuous, dull ache that wraps around both sides of the head.
- *Sensation:* The sensation is often likened to a tight band encircling the forehead, creating a sensation of pressure.
- *Duration:* These headaches can occur episodically, triggered by specific stressors, or transition into a chronic state, persisting for extended periods.
- *Description:* Migraines are characterized by intense, throbbing pain that may be localized to one side of the head.
- *Intensity:* The pain is often severe, impacting daily activities and requiring individuals to seek relief in a quiet, darkened environment.
- *Nausea and Vomiting:* Migraines may be accompanied by nausea, sometimes leading to vomiting, exacerbating the overall discomfort.
- *Sensitivity to Light and Sound:* Exposure to bright lights and loud noises intensifies migraine symptoms.
- *Visual Disturbances:* Some individuals experience visual auras, seeing flashes of light or zigzag patterns, preceding the onset of the migraine.
- *Prodrome:* Before the onset, individuals may experience subtle signs such as mood changes, food cravings, or increased yawning.
- *Postdrome:* Following the resolution of the migraine, a postdrome phase may bring about fatigue, confusion, and a lingering sense of unwellness.
Understanding the nuanced symptoms of tension-type headaches and migraines is pivotal for accurate diagnosis and tailoring effective treatment plans. Individuals experiencing these symptoms should seek professional medical advice to explore appropriate interventions and improve their overall quality of life.
- *Contributing Factors:* The primary instigators of tension-type headaches often stem from heightened stress levels and resulting muscle tension in the neck and scalp.
- *Physiological Response:* Prolonged stress triggers the tightening of muscles, creating a constrictive sensation that evolves into persistent tension headaches.
- *Impact:* Incorrect posture, particularly during prolonged periods of sitting or computer use, contributes to muscle strain in the neck and upper back.
- *Alignment Disturbances:* Poor posture disrupts the natural alignment of the spine, becoming a catalyst for tension headaches.
- *Role:* Emotional factors, such as anxiety and emotional stress, significantly contribute to the onset of tension-type headaches.
- *Psychophysiological Connection:* The intricate interplay between emotional well-being and physical manifestations underscores the psychophysiological nature of these headaches.
- *Triggers:* Migraines in some individuals are intricately linked to hormonal fluctuations, particularly prevalent during menstruation, pregnancy, or hormonal medication use.
- *Sensitivity to Hormones:* Sensitivity to hormonal changes underscores the complex hormonal triggers associated with migraines.
- *Triggers:* Certain foods and beverages act as triggers for migraines in susceptible individuals. These may include aged cheese, chocolate, caffeine, and alcohol.
- *Metabolic Response:* The intricate interplay between dietary elements and metabolic processes contributes to the initiation of migraines.
- *Triggers:* Migraines can be provoked by exposure to bright lights, loud sounds, and strong odors, emphasizing the role of sensory stimuli.
- *Neurological Sensitivity:* The heightened sensitivity of the nervous system to external stimuli amplifies the impact of sensory triggers.
- *Association:* Emotional stress and changes in routine serve as prominent triggers for migraines.
- *Neurovascular Mechanisms:* Stress-induced neurovascular changes contribute to the initiation and escalation of migraine attacks.
- *Role:* Irregular sleep patterns, insufficient sleep, or excessive sleep can disrupt the delicate balance, acting as triggers for migraines.
- *Circadian Rhythm Impact:* The intricate relationship between sleep, circadian rhythms, and migraine pathophysiology underscores the multifactorial nature of migraine causation.
Understanding the intricate causes of tension-type headaches and migraines is essential for developing targeted interventions. By recognizing the diverse physiological and psychosocial elements at play, healthcare professionals can formulate comprehensive strategies that address the root causes of cranial pain.
1. Musculoskeletal Assessment:
- *Initial Step:* Osteopathic treatment begins with a thorough musculoskeletal assessment, targeting areas of tension, misalignment, or dysfunction that may contribute to headaches.
2. Manual Techniques:
- *Soft Tissue Manipulation:* Osteopaths employ hands-on techniques to release tension in muscles, especially in the neck and upper back, aiming to alleviate stress contributing to headaches.
3. Cranial Osteopathy:
- *Focus:* Cranial osteopathy involves gentle manipulation of the skull, spine, and sacrum, addressing imbalances in the craniosacral system, potentially easing headache symptoms.
4. Postural Advice:
- *Guidance:* Osteopaths provide guidance on improving posture, which can help prevent the recurrence of tension-type headaches related to musculoskeletal strain.
1. Exercise Therapy:
- *Strengthening Exercises:* Physiotherapists prescribe targeted exercises to strengthen the muscles in the neck and shoulders, addressing underlying issues contributing to tension headaches.
2. Stretching Exercises:
- *Flexibility Enhancement:* Specific stretches can improve flexibility and reduce muscle tightness, particularly in areas prone to tension and trigger points.
3. Ergonomic Advice:
- *Workstation Assessment:* Physiotherapists assess workstations and provide advice on ergonomics, ensuring proper posture and reducing strain during daily activities.
4. Joint Mobilization:
- *Techniques:* Physiotherapists may use joint mobilization techniques to enhance the mobility of the cervical spine, addressing stiffness that could contribute to headaches.
5. Education and Lifestyle Modifications:
- *Holistic Approach:* Physiotherapists educate individuals on lifestyle modifications, stress management techniques, and relaxation exercises to prevent headache recurrence.
- *Tailored Approach:* Osteopathic and physiotherapeutic interventions are tailored to the individual, considering the specific characteristics and triggers of their headaches.
- *Team Approach:* Collaborative care involving osteopathy, physiotherapy, and other healthcare professionals ensures a holistic approach to managing headaches.
- *Long-Term Management:* Osteopathy and physiotherapy focus not only on alleviating current symptoms but also on implementing preventive strategies to reduce the frequency and intensity of headaches.
- *Education and Self-Care:* Both osteopathy and physiotherapy empower individuals through education, emphasizing self-care strategies and lifestyle modifications to manage and prevent headaches independently.
The journey through the realm of migraines and headaches concludes with a nuanced understanding that extends beyond the immediate discomfort. As we traverse this intricate landscape, the recognition of diversity in symptoms, triggers, and impacts becomes paramount. This conclusion serves as a compass, guiding individuals, healthcare professionals, and researchers toward comprehensive approaches to managing and mitigating the complexities of cranial pain.
1. Holistic Management:
- *Beyond Symptomatic Relief:* Acknowledging migraines and tension-type headaches as intricate conditions demands a holistic approach that transcends symptomatic relief.
- *Comprehensive Strategies:* Comprehensive management involves addressing the multifaceted interplay of physiological, psychological, and environmental factors contributing to cranial pain.
2. Empowering Individuals:
- *Educational Empowerment:* Empowering individuals with knowledge about their specific condition fosters a sense of agency and control over their well-being.
- *Lifestyle Modification:* Encouraging lifestyle modifications, stress management techniques, and self-care practices equips individuals with tools for ongoing cranial health.
3. Collaborative Care:
- *Integrated Healthcare:* The complexities of migraines and tension-type headaches underscore the significance of collaborative care.
- *Interdisciplinary Approach:* An integrated approach involving healthcare professionals from diverse fields ensures a comprehensive understanding and management of cranial pain.
4. Research Frontiers:
- *Unraveling Complexity:* Ongoing research endeavors continue to unravel the intricate intricacies of migraines and tension-type headaches.
- *Innovation in Care:* Advances in understanding the genetic, neurobiological, and environmental factors contributing to these conditions pave the way for innovative care modalities.
5. Patient-Centric Approach:
- *Tailored Care Plans:* Recognizing the uniqueness of each individual's experience is foundational to crafting tailored care plans.
- *Patient Involvement:* Involving patients as active participants in their healthcare journey fosters a sense of partnership and enhances the effectiveness of interventions.
In conclusion, the journey through migraines and headaches transcends the immediate sensations, offering an opportunity for empowerment, collaboration, and innovation. As we navigate this complex landscape, the commitment to ongoing research, patient-centric care, and holistic strategies ensures that individuals grappling with cranial pain find solace in a future where the intricacies of their experience are met with compassion, understanding, and effective management.
Achilles tendinitis is a prevalent overuse injury that impacts the Achilles tendon—a critical band of tissue that connects the calf muscles to the heel bone.
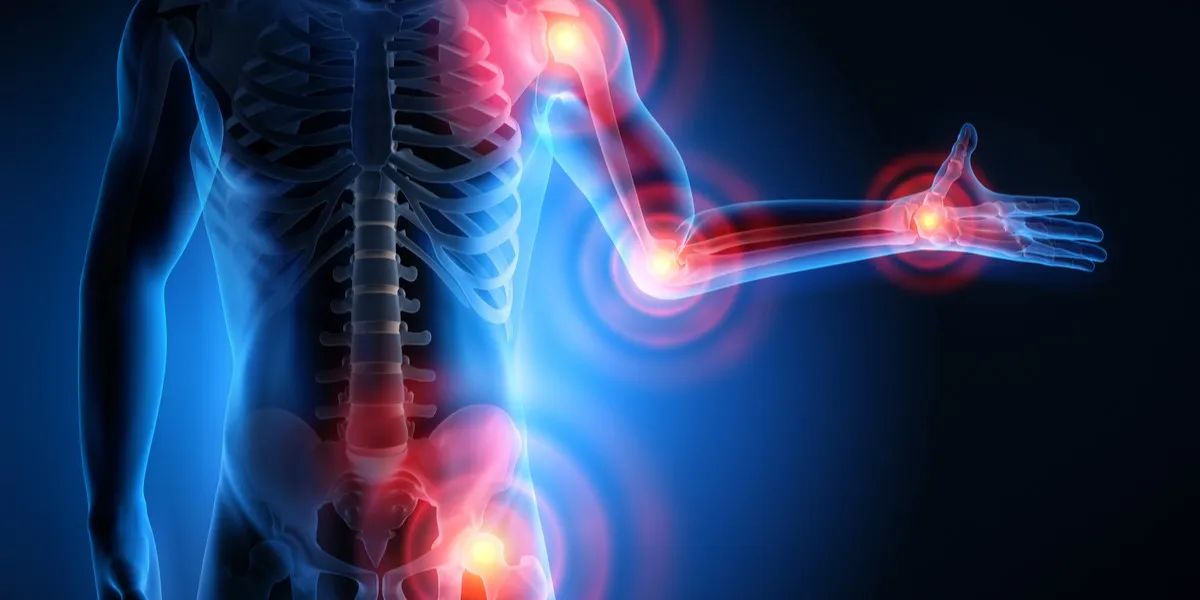
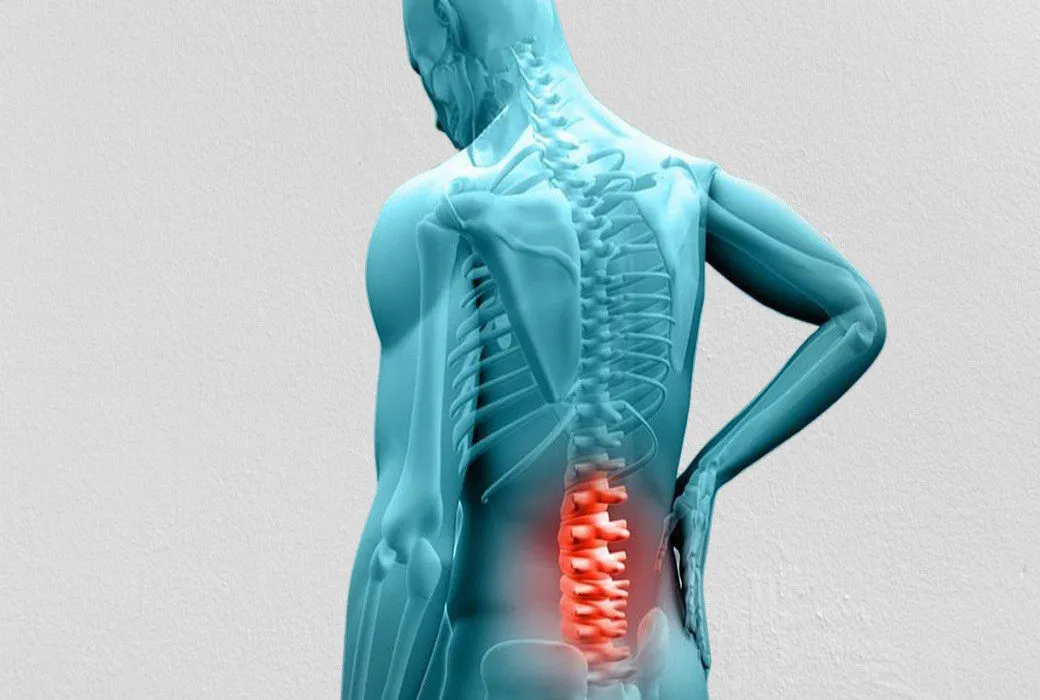
Back pain is a prevalent and often debilitating condition that can affect individuals of all ages and walks of life.

Arthritis is a common and often painful condition that affects millions of individuals worldwide. It's not a single disease but rather a group of more than 100 different types of joint-related conditions.
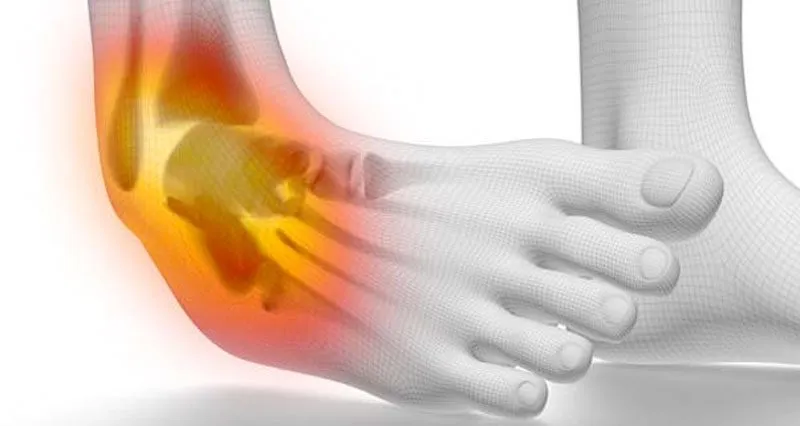
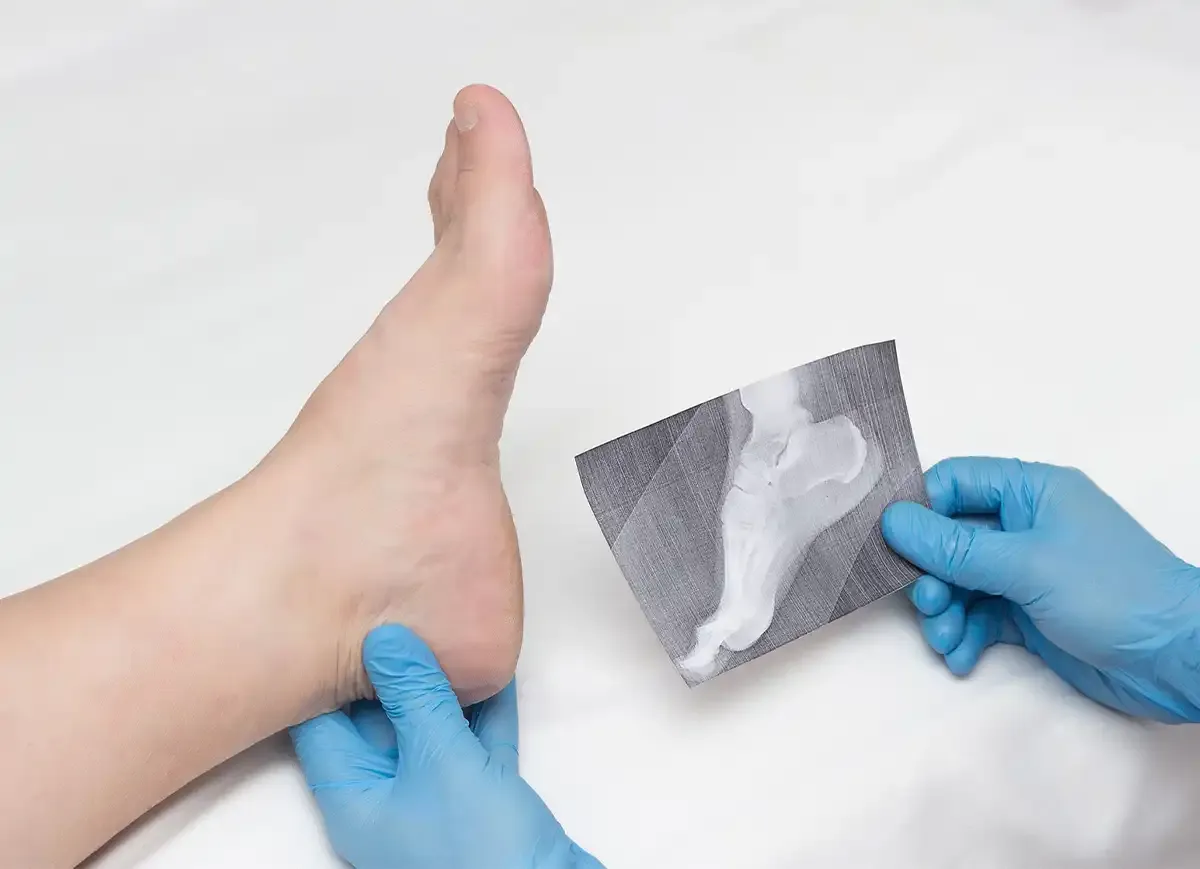
Ankle injuries are prevalent in the world of sports and can be a significant setback for athletes.
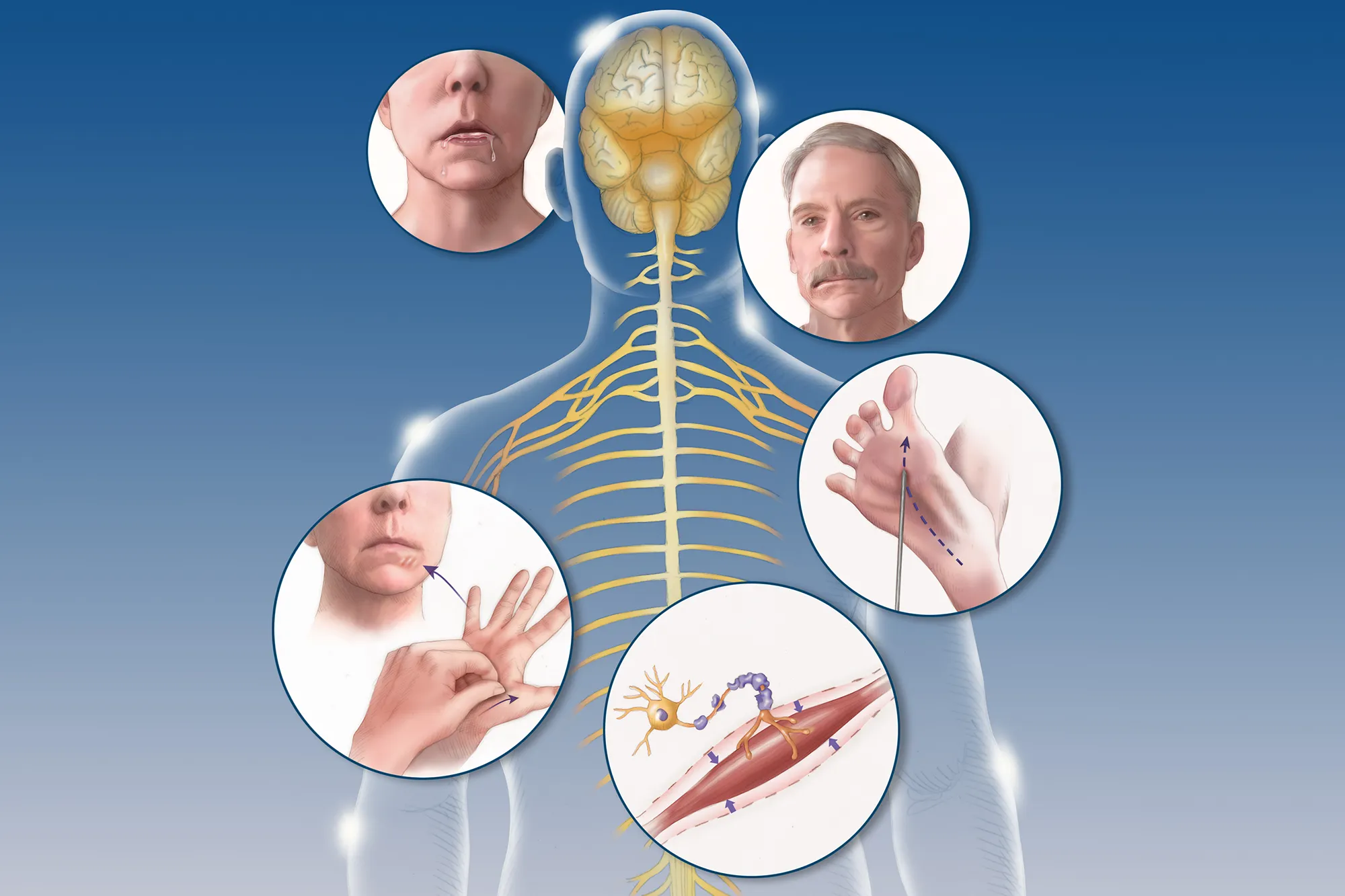
Amyotrophic Lateral Sclerosis (ALS), often referred to as Lou Gehrig's disease, is a progressive neurodegenerative disorder that affects nerve cells in the brain and spinal cord.
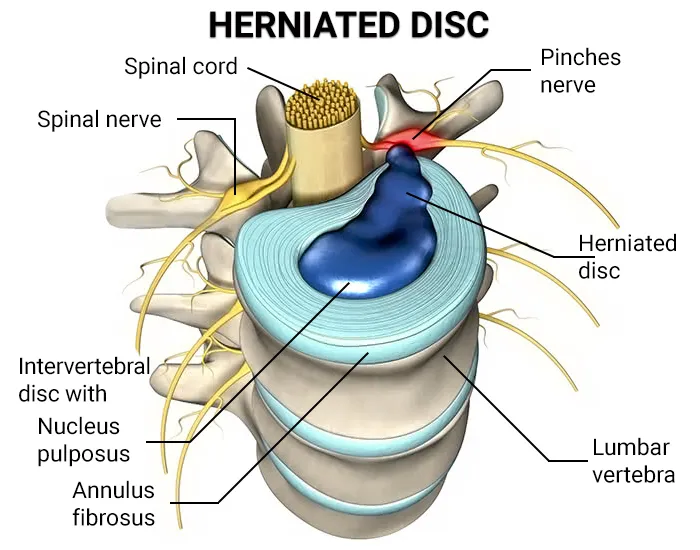
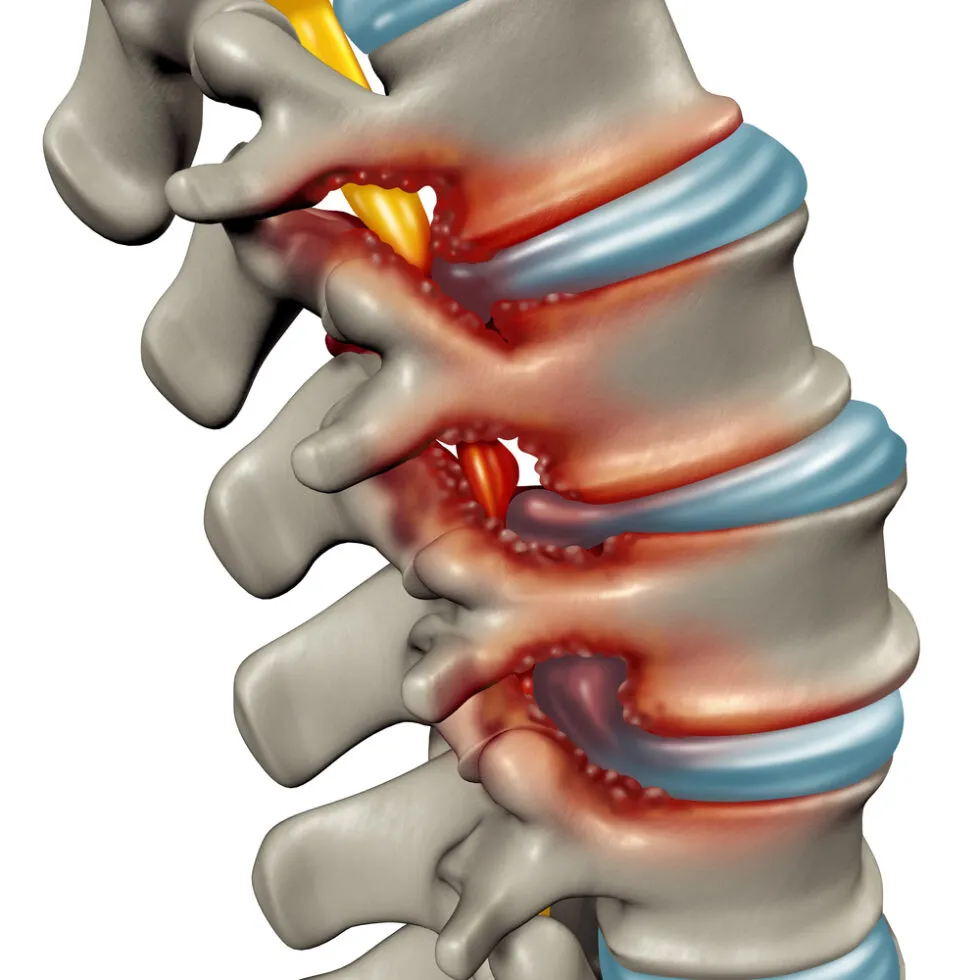
Degenerative Disc Disease (DDD) is a common condition that affects the intervertebral discs in the spine.
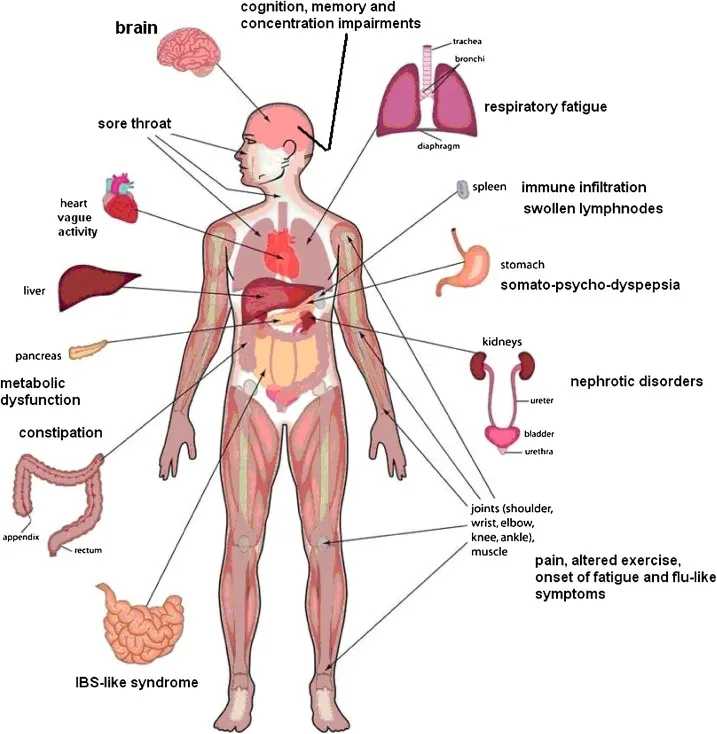
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is a perplexing and debilitating condition that impacts individuals, often altering their daily lives and challenging conventional understanding.
Muscular dystrophy encompasses a group of diseases leading to progressive muscle weakness and loss of muscle mass. The development of abnormal genes disrupts the production of necessary proteins crucial for healthy muscle function.

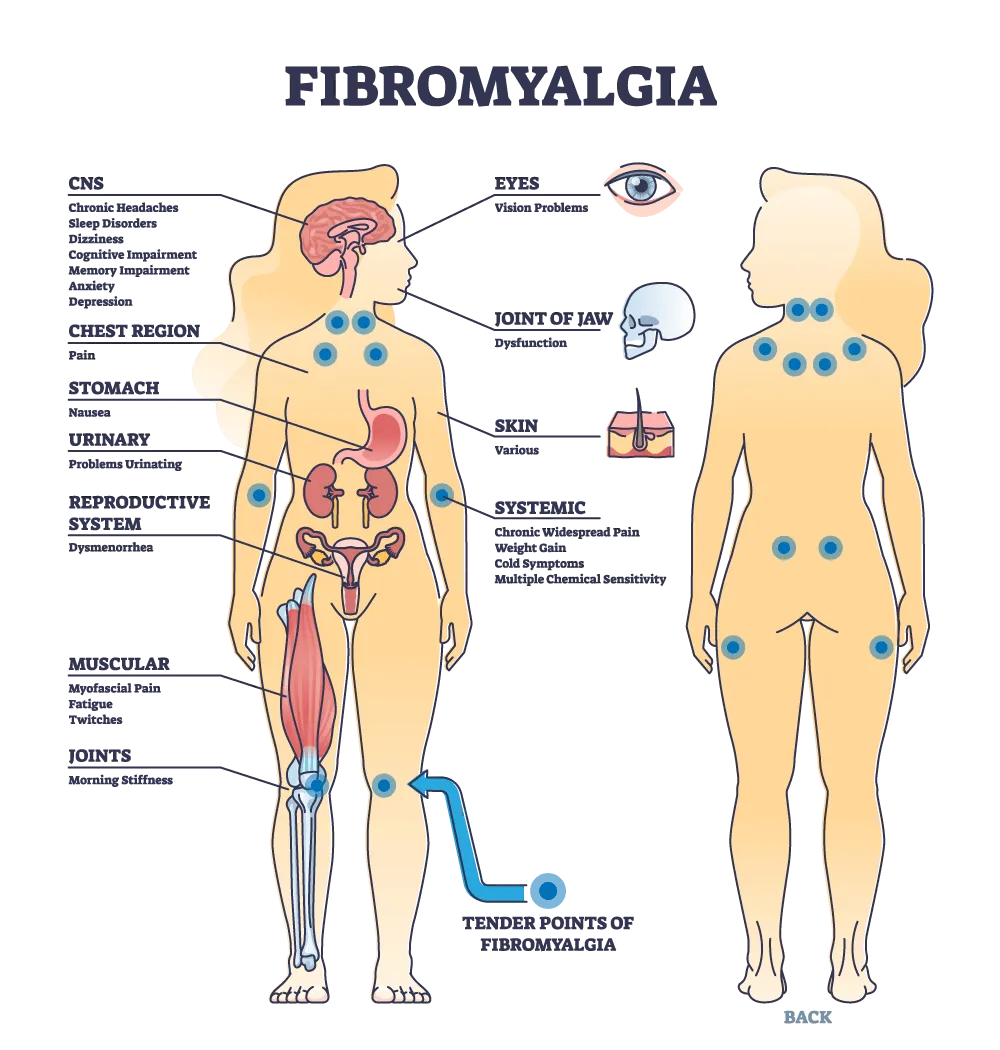
Fibromyalgia stands as a complex and often misunderstood condition characterized by widespread musculoskeletal pain, fatigue, and sleep disturbances
Bunions, medically referred to as "hallux valgus," are a common and often painful foot deformity that affects the joint at the base of the big toe.

Herniated disc symptoms can be debilitating, causing pain, numbness, and mobility limitations.
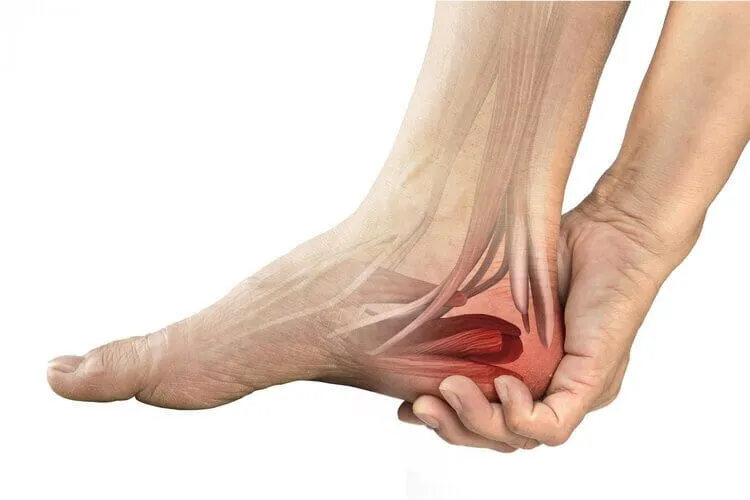
A heel spur is a bony growth that pokes out below your back heel bone inside of your foot. Heel spurs happen when stress and strain damages your foot ligaments.
Knee pain is a widespread issue that can significantly impact a person's mobility and quality of life.Knee pain is a widespread issue that can significantly impact a person's mobility and quality of life.

Heel pain can be a nagging and uncomfortable issue that affects many people. In this article, we will explore the various causes of heel pain, common symptoms associated with it, and the available treatments that can help you find relief and get back to your active lifestyle.
Military Neck, also referred to as Cervical Kyphosis, is a condition that affects the natural curvature of the cervical spine, resulting in the loss of its typical curve.

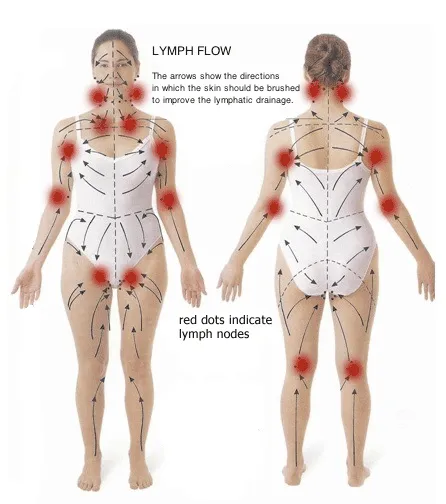
Lymphedema is a chronic condition characterized by the accumulation of lymphatic fluid, leading to persistent swelling, typically in the arms or legs.
Plantar fasciitis is a common and often painful foot condition that affects millions of people worldwide.

Piriformis syndrome is a perplexing condition, often overshadowed by more common sources of hip and lower back pain.

motor vehicle accidents (MVA) can result in a wide range of injuries, from minor bruises to severe trauma. in the aftermath of such incidents, seeking prompt medical attention is crucial for assessing and addressing any injuries sustained.

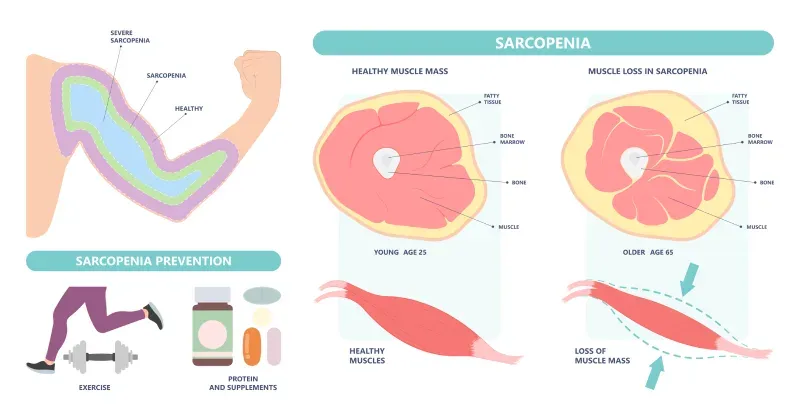
Sarcopenia is the gradual loss of muscle mass that can affect people in their 30s and beyond. WebMD explains its symptoms, causes, diagnosis, and treatments.
Spinal stenosis, a prevalent spinal condition, is characterized by the narrowing of the spinal canal, leading to discomfort and neurological symptoms.
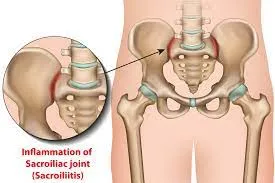
The sacroiliac joint, a crucial junction between the sacrum and the ilium bones in the pelvis, plays a pivotal role in supporting the weight of the upper body.
A rotator cuff injury can be a painful and limiting condition, impacting the functionality of the shoulder.

Suffering from lower back pain from sitting? It could be from poor ergonomics in your workplace. Learn more with these tips for how to alleviate pain from sitting.

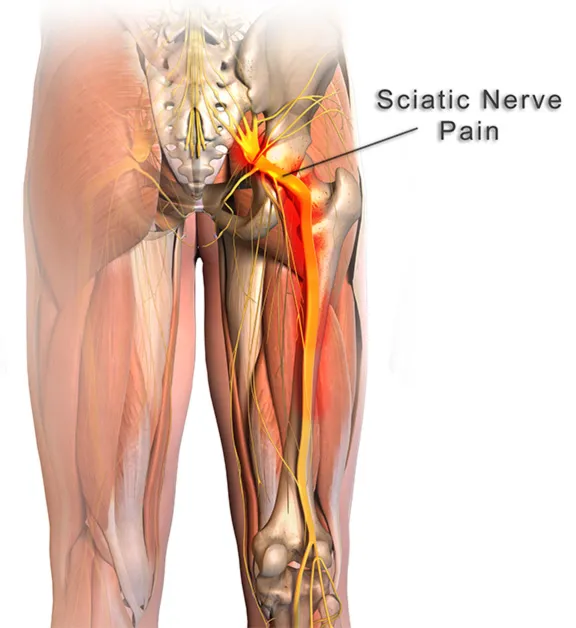
Sciatica is a painful and often debilitating condition that affects numerous individuals worldwide.
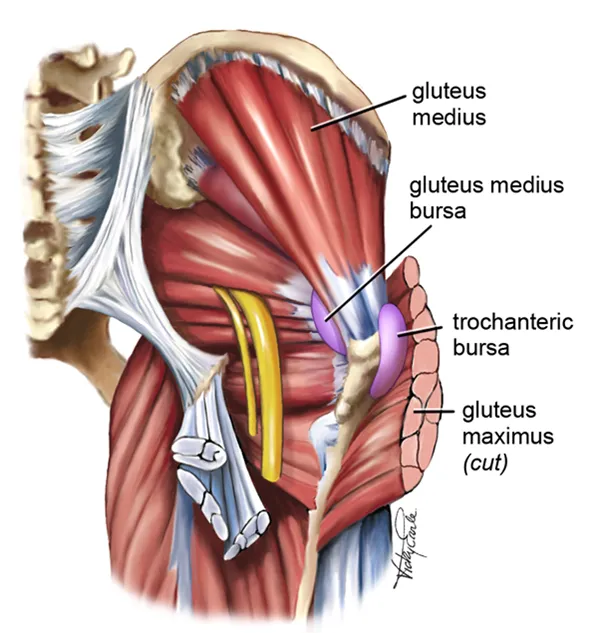
Gluteal tendinopathy is a condition that affects the tendons in the gluteal region, leading to pain and restricted mobility.
Tennis Elbow, also known as Lateral Epicondylitis, is a painful condition that affects the tendons in the forearm, causing discomfort and limited mobility in the elbow and wrist.

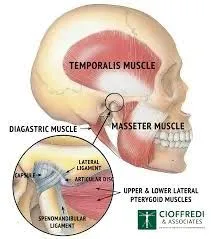
The temporomandibular joint (TMJ) serves as a pivotal mechanism, allowing us to perform everyday activities such as speaking, chewing, and yawning with ease. However, when this complex joint encounters issues, it can lead to Temporomandibular Joint Syndrome (TMJ syndrome).
Tarsal Tunnel Syndrome (TTS) is a common and often painful condition affecting the tarsal tunnel—a narrow passage in the ankle.

Explore the impact of time-restricted eating on heart health. Learn about the connection between diet and cardiovascular risk.

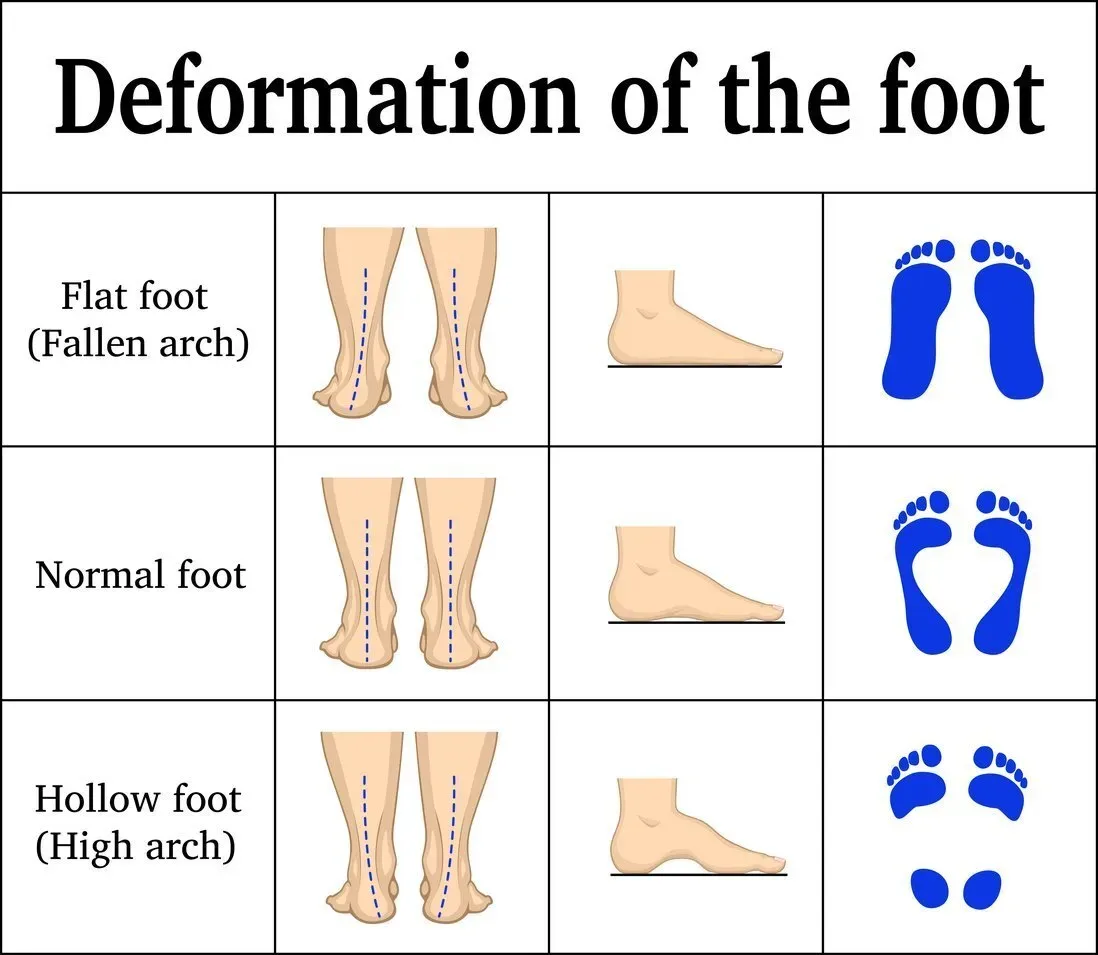
Most cases of foot or ankle pain are short term and are caused by soft tissue injuries, such as sprains or strains. You can usually ease the pain yourself But see York Rehab Clinic if the pain does not improve.

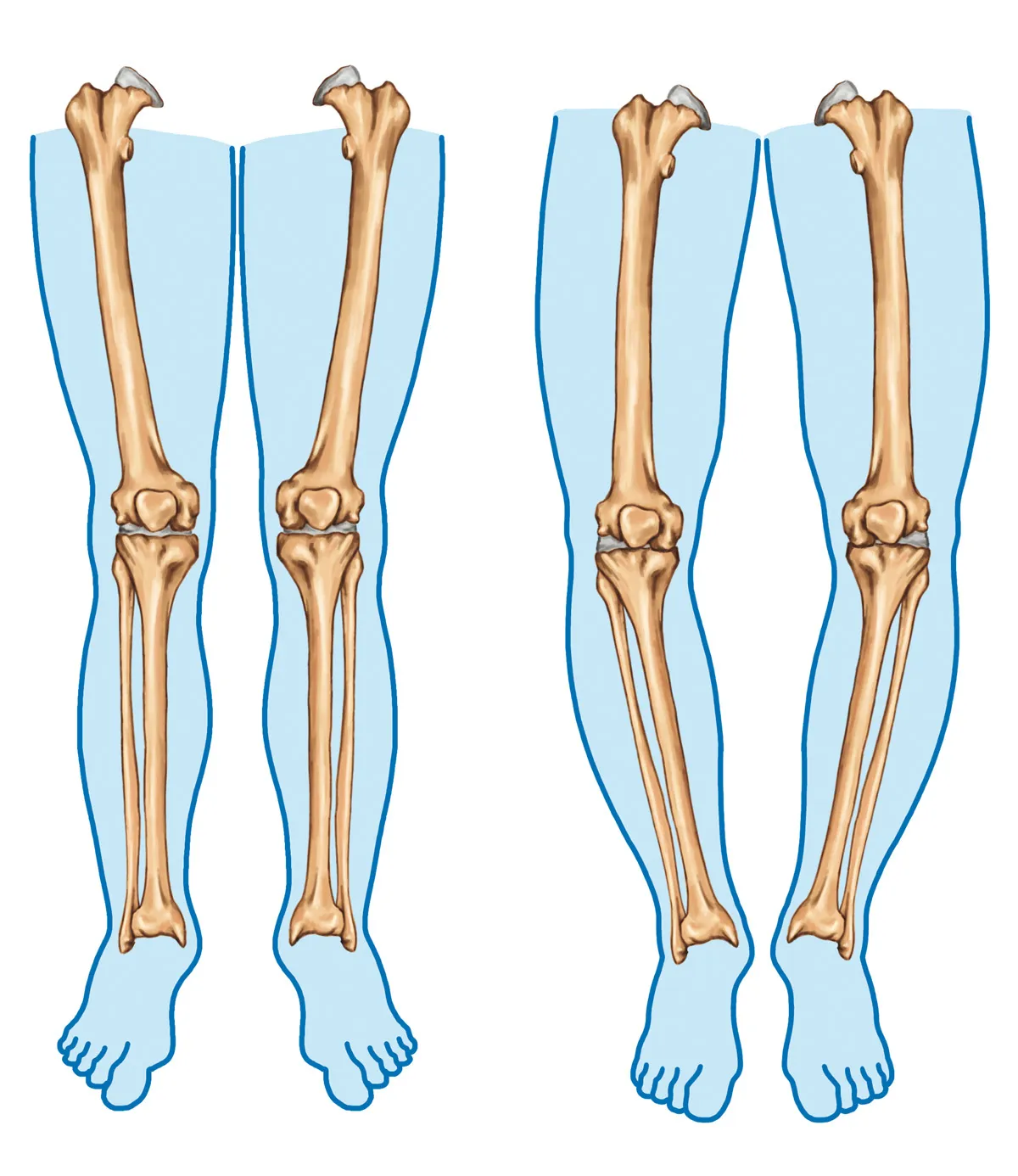
Bow legs is a genetic condition where the knees bow outward when standing. Learn its symptoms and causes at York Rehab Clinic.
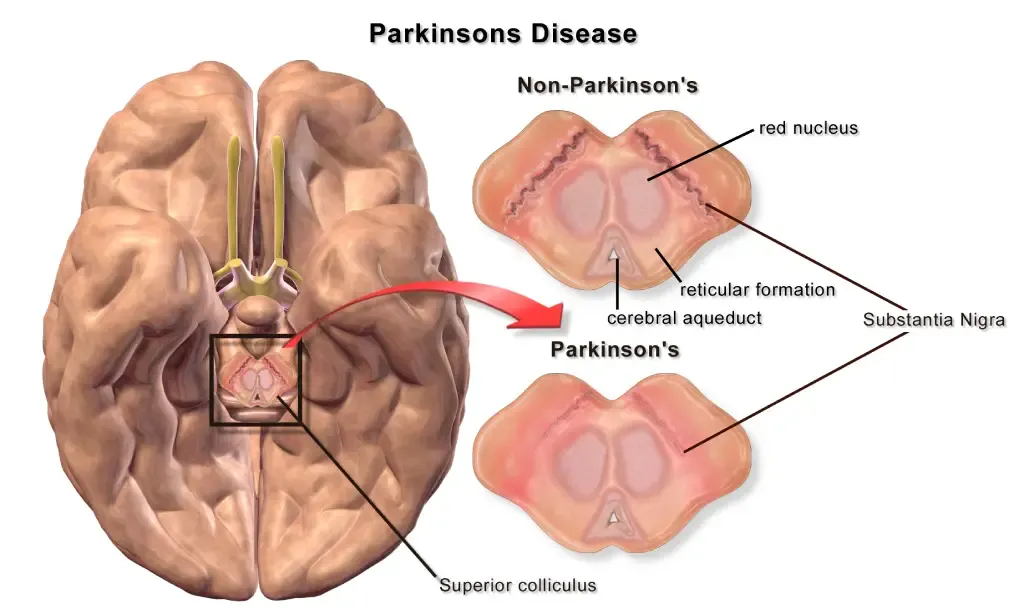
This article explores the complexities of Parkinson’s Disease and sheds light on the therapeutic benefits offered by osteopathy and physiotherapy.
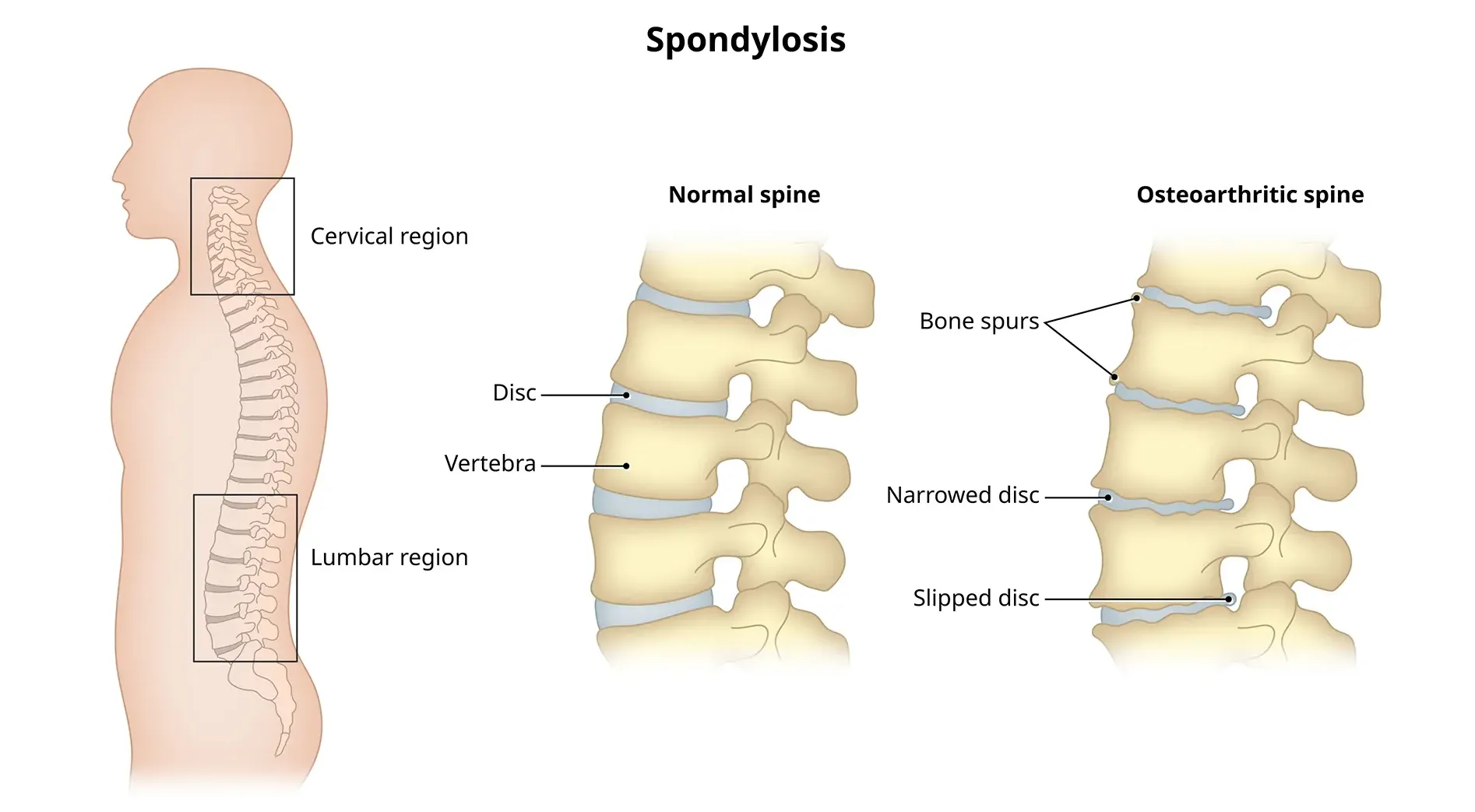
Cervical spondylosis, a prevalent condition, unfolds as a result of wear and tear on the spinal discs in the neck.
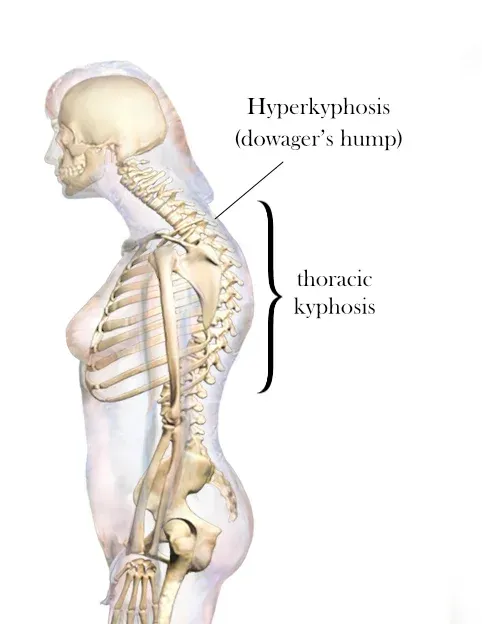
A dowager’s hump, a curve at the base of your neck, can cause extreme fatigue, back pain and headaches.
Flat feet cause pain, muscle strain, and fatigue. Treatments can ease discomfort. Symptoms include ankle pain, muscle fatigue and changes in walking.
Traumatic brain injury (TBI) often results from a violent blow or jolt to the head or body, causing various physical and psychological effects.

Introduction: Neck stiffness can be a discomforting and limiting condition that affects people of all ages.
