25% off valentine’s day for specialist treatments
Book your initial visit online and enjoy 25% off on our expert osteopathic, physiotherapy, and acupuncture services.
July 30, 2023, 5 min read, Other
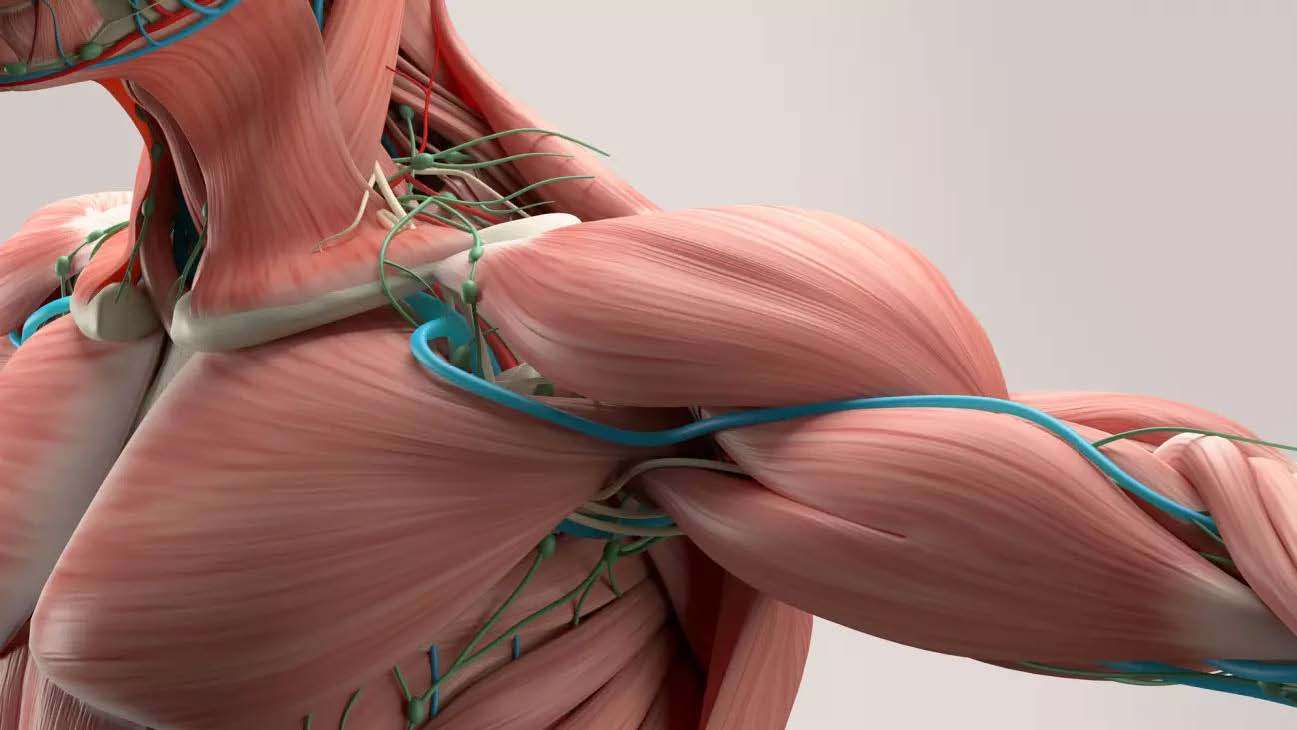
Thoracic outlet syndrome (TOS) is a group of disorders that occur when blood vessels or nerves in the space between your clavicle and your first rib (thoracic outlet) are compressed. This can cause shoulder and neck pain and numbness in your fingers.
Common causes of thoracic outlet syndrome include physical trauma from a car accident, repetitive injuries from job- or sports-related activities, certain anatomical defects (such as having an extra rib), and pregnancy. Sometimes doctors don’t know the cause of thoracic outlet syndrome.
Neurogenic TOS is characterized by compression of the brachial plexus, a network of nerves that run from your spinal cord to your upper limbs and control muscle movements and sensation in your shoulders, arms, and hands. Neurogenic TOS can result in tingling, weakness, and even mild skin color changes when you raise your arms overhead. This is the most common type of TOS in adults.
Venous TOS happens when the vein that drains blood from the arm, the subclavian vein is compressed as it travels under the clavicle and through the thoracic outlet. This can cause swelling, and redness or make your arm feel heavy when you use it or raise it overhead. In extreme cases, venous TOS can cause clotting of the vein, resulting in significant swelling and persistent pain. This situation is called effort thrombosis, or Paget-Schroetter disease. This type of TOS often affects children.
Arterial TOS occurs when the muscles and bones surrounding the thoracic outlet rub against (impinge) the subclavian artery, the artery that supplies blood to the arm. This can result in loss of blood flow to the arm and make your arm feel cold and painful. Often this is temporary, happening only when your arm is raised. However, severe or long-term arterial TOS can damage the artery, cause clotting and require emergency medical attention. The rarest form, arterial TOS, requires surgery to decompress the thoracic outlet.
With proper treatment, TOS is a manageable condition. Although many cases of thoracic outlet syndrome are not preventable, the condition is treatable. Treatment is important to prevent serious complications. If left untreated, TOS can cause complications, such as:
It’s possible to have a mix of the three different types of thoracic outlet syndrome, with multiple parts of the thoracic outlet being compressed. Thoracic outlet syndrome symptoms can vary depending on the type. When nerves are compressed, signs and symptoms of neurogenic
Thoracic outlet syndrome is usually caused by compression of the nerves or blood vessels in the thoracic outlet, just under your collarbone (clavicle). The cause of the compression varies and can include:
Several factors seem to increase the risk of thoracic outlet syndrome, including:
If you’re at risk for thoracic outlet compression, avoid repetitive movements and lifting heavy objects. If you’re overweight, losing weight may help you prevent or relieve symptoms of thoracic outlet syndrome. Even if you don’t have symptoms of thoracic outlet syndrome, avoid carrying heavy bags over your shoulder, because this can increase pressure on the thoracic outlet.
Stretch daily, and perform exercises that keep your shoulder muscles strong. Daily stretches focusing on the chest, neck, and shoulders can help improve shoulder muscle strength and prevent thoracic outlet syndrome.
Proper diagnosis is the most important step in treating thoracic outlet syndrome. Your doctor will perform a complete physical exam and review the results of previous diagnostic tests. Your doctor may recommend a thorough evaluation by a skilled neurologist to rule out cervical spine disease and other neurological conditions with similar symptoms.
Additional tests that help diagnose thoracic outlet syndrome include:
Proper diagnosis is the most important step in treating thoracic outlet syndrome. Your doctor will perform a complete physical exam and review the results of previous diagnostic tests.
Most cases of neurogenic thoracic outlet syndrome can be treated with physical therapy and medication. Severe cases may require surgery.
Osteopathy, Chiropractic and physiotherapy can help to treat patients by applying Electro therapy, Manual therapy, and a variety of exercises that effectively stretch open the tissues of the thoracic outlet. These are done with and without weights to pull the outlet into a “relaxed” open position. Physical therapy may be done before surgery, as in the case of neurogenic TOS, or may be prescribed after surgery to help you regain strength and stability.
Your doctor might prescribe medications such as anti-inflammatory medications (ibuprofen, Advil) or muscle relaxants to help relieve your symptoms. Cortisone injected into a joint or muscle can help lower inflammation and provide relief. If you have venous or arterial TOS, your doctor may prescribe blood thinners to prevent or treat blood clots.
Our goal in the Thoracic Outlet Syndrome Program is to return our patients to full function, This requires varying levels of intervention. York rehab Clinic has an extensive team of Osteopathy, Chiropractic, Physiotherapy, Massage therapy and Acupuncture to help you.
Call to us at 416-350-1940 to make your appointment.
Book your initial visit online and enjoy 25% off on our expert osteopathic, physiotherapy, and acupuncture services.

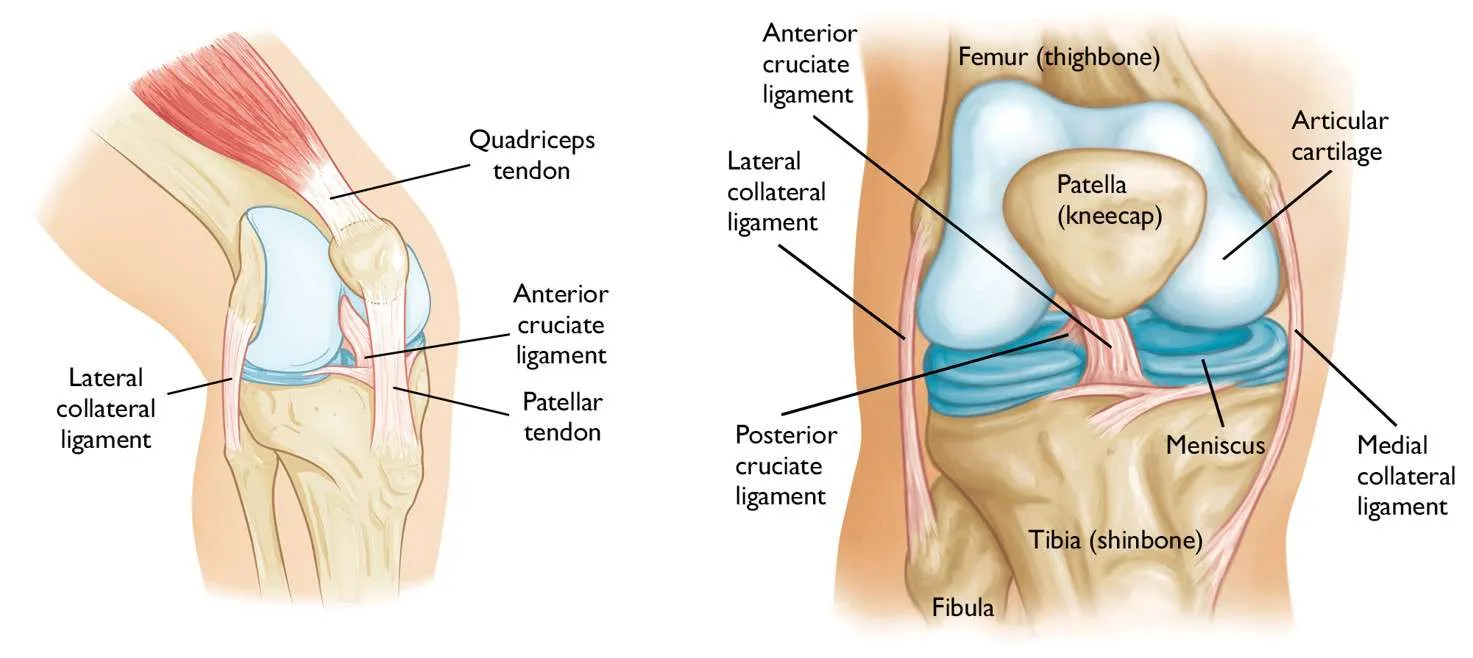
Knee injuries are particularly common among athletes. In 2010, more than 10 million people visited a doctor because of pain or a knee injury.
When your feet are in pain it can have a pretty nasty effect on your everyday life.

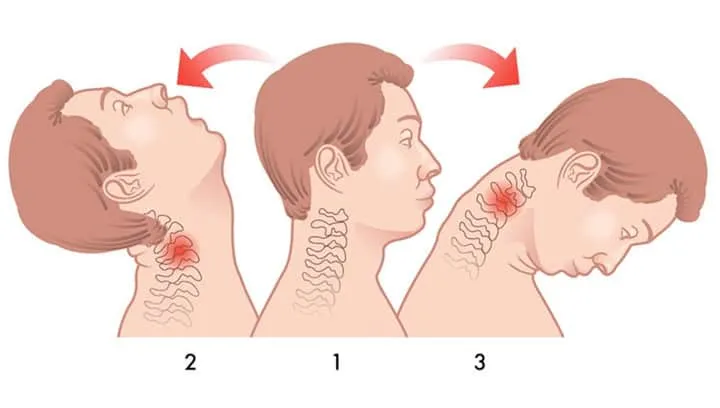
A healthy neck has a “C” curve (lordosis) when you see it from the side and the curve rolls forward from the bottom of the cervical spine and curves back again halfway up to the head. the healthy neck has approximately 30 to 40 degrees of the curve.

Whiplash is a neck injury caused by a sudden and violent movement of the head in one direction and then quickly back again, usually during a car accident.
As the cold season rolls around, so do it’s many changes in atmosphere and overall energy.

Happy Nowruz from all of us at York Rehab Clinic!🎉
130 years after the founding of the American School of Osteopathy, Andrew Taylor Stills’s contribution is keeping osteopathic research and practice alive.